Mastering Physiological Adaptation for the NCLEX‑RN® (2025 Update)
Introduction
Physiological adaptation questions make up 11 %–17 % of the NCLEX‑RN® test plan—and 2025 adds heavier emphasis on trend analysis and Next‑Generation NCLEX (NGN) case studies. This fully revised guide delivers blueprint changes, high‑yield mnemonics, evidence‑based interventions, and direct practice links so you can convert one of the toughest categories into easy points.
1. 2025 NCLEX Blueprint & Weighting
| Client‑Needs Category | NCLEX Weight | Core Focus |
|---|---|---|
| Physiological Adaptation | 11 %–17 % | Hemodynamics • Acid‑base • Neuro emergencies • Acute/Chronic illness |
Source: NCSBN NCLEX‑RN Test Plan (.org)
2025 Highlights
- Guaranteed 3 NGN case studies—expect at least one physiological scenario.
- Greater emphasis on early deterioration recognition (serial vitals, labs).
- Partial‑credit items reward evidence‑based priorities.
2. Core Concepts You Must Own
2.1 Cardiovascular Hemodynamics
| Parameter | Normal | Rationale |
|---|---|---|
| MAP | ≥ 65 mm Hg | Maintains organ perfusion |
| Cardiac Output (CO) | 4–8 L/min | Gauges pump efficiency |
| Central Venous Pressure | 2–6 mm Hg | Guides fluid resuscitation |
Mnemonic—“FLOOD” Shock Algorithm
Fluids → Levophed → Oxygen → Optimize position → Diagnose cause
Internal read: NCLEX Prep: Fluid & Electrolytes Guide
2.2 Acid‑Base & Respiratory Management
- Metabolic Acidosis (DKA): Rapid IV fluids + insulin; add bicarbonate if pH < 7.0.
- Respiratory Alkalosis (early sepsis): Coach slow breathing; treat infection.
2.3 Neuro & Increased Intracranial Pressure (ICP)
“PRESS” Algorithm
- Position HOB 30°
- Resp CO₂ 35–40 mm Hg
- Evaluate pupils & GCS hourly
- Sedate to curb agitation
- Stool softeners—avoid Valsalva spikes
Internal read: Delirium Tremens NCLEX Guide
2.4 Endocrine & Electrolyte Emergencies
| Crisis | First‑Line Treatment | NCLEX Pearl |
|---|---|---|
| Thyroid storm | PTU → Iodine → Beta‑blocker | Beta‑blockers blunt SNS surge |
| Myxedema coma | IV Levothyroxine + gentle warming | Rapid warming → vasodilation shock |
| Tumor‑lysis syndrome | Hydration, allopurinol, rasburicase | Monitor Ca²⁺, K⁺, uric acid |
3. High‑Yield Mnemonics & Memory Aids
- CAKE (hyperkalemia ECG): C Peaked T, A Absent P, K Wide QRS, E Sine wave
- “Cool & Clammy → Need Candy” for hypoglycemia
- FAST HUGS BID (Feeding, Analgesia, Sedation, Thrombo‑prophylaxis, etc.) for daily ICU checks
For terminology drill, see 25 Essential Words to Know Before the NCLEX.
4. NGN Case‑Based Question Strategy
Layered‑Cue Framework
- Frame the scenario (acute vs. chronic).
- Filter trend data (vitals, labs).
- Focus on the intervention that halts decline fastest.
Partial‑credit tip: Eliminate harmful actions first—each safe choice earns points.
5. Four‑Week Study Plan
| Day | Focus Area | Resource |
|---|---|---|
| Mon | Hemodynamics & shock | Fluid & Electrolytes Guide |
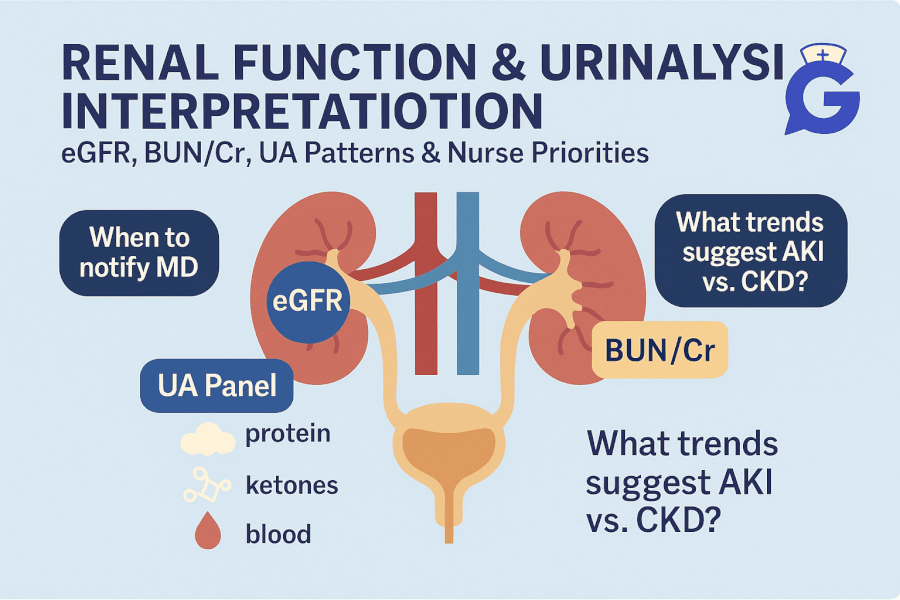
| Tue | Acid‑base interpretation | Quiz bank |
| Wed | Neuro & ICP | Delirium Tremens Guide |
| Thu | Endocrine crises + electrolytes | Flashcards |
| Fri | Mixed Med‑Surg NGN set | 75‑Q block |
| Sat | Review weak metrics | Personal notes |
| Sun | Full‑length adaptation quiz | See call‑out |
6. Call‑Out: Are You Ready?
🎯 Free NCLEX quiz!
Test your knowledge, we're always adding more quizzes!.
7. Authoritative External Resources
- NCSBN NCLEX‑RN Test Plan (.org)
- MedlinePlus: Critical Care (.nih.gov)
- West Coast University Library Guide (.edu)
8. Key Takeaways
- Trend recognition beats isolated numbers—watch MAP, CO, serial labs.
- Mnemonics like FLOOD and PRESS streamline emergency priorities.
- Consistent NGN practice plus GoodNurse quizzes close final knowledge gaps.