I. Introduction: Why Mastering NCLEX Pharmacology Is Crucial for Your Success
Pharmacology is not merely another subject to study for the National Council Licensure Examination (NCLEX); it stands as a fundamental pillar of the exam and, more importantly, of safe and effective nursing practice. A substantial portion of the NCLEX—specifically 13–19 % for NCLEX‑RN candidates—is dedicated to Pharmacological and Parenteral Therapies. This significant weighting underscores the critical need for aspiring nurses to achieve a robust understanding of medications, their actions, and their implications for patient care. Success in this area is directly linked to success on the NCLEX and lays the groundwork for a career centered on patient safety.
🎯 Free NCLEX quiz on this topic!
Test your knowledge after you finish reading.
Many nursing students find pharmacology to be one of the most challenging aspects of their curriculum, often feeling overwhelmed by the sheer volume of drug names, mechanisms, side effects, and calculations. This guide is designed to bridge that gap, transforming complex pharmacological concepts into understandable and manageable information. The aim is to demystify the subject—true to the “Made Simple” promise—empowering you to approach the NCLEX with confidence.
This ultimate guide will serve as your roadmap to mastering NCLEX pharmacology. It will navigate through foundational principles—what the body does to a drug (pharmacokinetics) and what a drug does to the body (pharmacodynamics). It will simplify drug‑dosage calculations, provide clear formulas and practical tips, and delve into high‑yield drug classifications frequently encountered on the NCLEX, emphasizing essential nursing considerations. Crucially, medication safety—a non‑negotiable aspect of nursing—will be a recurring theme, alongside effective study strategies tailored for pharmacology.
Understanding the “why” behind the “what” is paramount. The NCLEX is designed to assess your ability to provide safe and effective care, and medication administration is a high‑risk nursing activity. A deep grasp of how drugs work, their potential side effects, interactions, and the mathematics behind correct dosing is not just about recalling facts for an exam; it is about ensuring patient well‑being. Therefore, this guide aims to instill not only the knowledge required to pass the NCLEX but also a profound appreciation for the critical role of pharmacology in daily nursing practice. Connecting theoretical knowledge with real‑world patient safety is the cornerstone of competent nursing.
II. The Building Blocks: Core Pharmacological Principles Explained
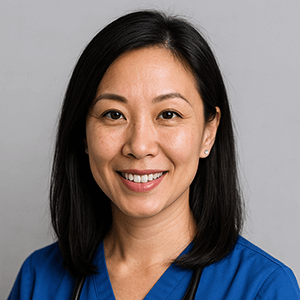
Before diving into specific medications, you need a solid understanding of how drugs interact with the human body. The two core principles—pharmacokinetics and pharmacodynamics—are the foundation upon which all other pharmacological knowledge is built. Mastering these concepts enables you to understand not just what drug to administer but why it works, how it might affect your patient, and what to watch for.
(Future GoodNurse cluster article: Core Pharmacological Principles)
A. Pharmacokinetics Made Simple: What the Body Does to the Drug (ADME)
Pharmacokinetics (PK) describes the journey a drug takes through the body—how it is Absorbed, Distributed, Metabolized, and Excreted (ADME). Understanding PK helps predict onset, peak, duration, and the risk of accumulation or toxicity; patient‑specific factors can alter every step.
(Future GoodNurse cluster article: Pharmacokinetics (ADME) for Nurses)
1. Absorption — Getting the Drug In
Absorption is the movement of a drug from its administration site into the bloodstream. The route dramatically affects speed and extent:
- Intravenous (IV): immediate, 100 % bioavailability
- Intramuscular (IM) / Subcutaneous (SQ): faster than oral, slower than IV
- Oral (PO): most common; variable, slower absorption
- Transdermal: slow, sustained systemic release
- Inhaled: rapid absorption via the lungs
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Key terms and factors:
- Bioavailability: fraction of the administered dose reaching systemic circulation unchanged
- First‑Pass Effect: oral drugs pass through the liver first, reducing active drug in circulation
- Factors influencing absorption: pH/lipid solubility, presence of food, local blood flow, drug formulation
2. Distribution — Getting the Drug Where It Needs to Go
Once in the bloodstream, drugs must reach target tissues:
- Protein Binding: only the unbound (“free”) fraction is active; low albumin ↑ free drug → toxicity risk
- Blood‑Brain Barrier: restricts many drugs from the CNS
- Tissue Perfusion: high‑flow organs (heart, liver, kidneys, brain) receive drugs fastest; dehydration or HF slows distribution
- Lipid Solubility: lipid‑soluble drugs cross membranes easily and may accumulate in fat
3. Metabolism — Breaking the Drug Down (Biotransformation)
Metabolism—mostly hepatic via the Cytochrome P450 system—chemically changes drugs, usually to water‑soluble forms for excretion.
- Liver & CYP450: genetic variations affect drug response
- Prodrugs: inactive until metabolized to active forms
- Half‑Life (t½): time for plasma concentration to drop 50 %; guides dosing intervals (steady state ≈ 4‑5 half‑lives)
- Enzyme Induction/Inhibition: some drugs speed up or slow down CYP450 activity, causing interactions
4. Excretion — Getting the Drug Out
Elimination of drugs and metabolites, primarily via the kidneys:
- Renal Excretion: impaired function → accumulation/toxicity; monitor creatinine, BUN, GFR
- Other Routes: bile/feces, lungs, sweat, saliva, breast milk
NCLEX Tip: Apply PK principles to practice—adjust doses for renal or hepatic impairment, consider albumin levels, time doses correctly, and teach patients about interactions.
B. Pharmacodynamics Made Simple: What the Drug Does to the Body
Pharmacodynamics (PD) looks at how a drug produces its effects—mechanisms, therapeutic outcomes, and adverse reactions.
Need a quick refresher on high‑yield meds?
Check out
NCLEX Pharmacology Made Easy: Must‑Know Drugs for 2025
—a concise rundown of drug classes you can’t afford to miss.
1. Mechanism of Action (MOA)
The biochemical interaction through which a drug produces its effect (e.g., receptor binding, enzyme inhibition).
2. Drug–Receptor Interactions — The Lock and Key
- Agonists: bind and activate receptors → response
- Antagonists: bind without activating, blocking agonists
- Affinity & Selectivity: strength of binding and preference for certain receptors; higher selectivity → fewer side effects
3. Therapeutic Effects — The Desired Outcomes
- Onset: time to first effect
- Peak: time to maximum effect
- Duration: how long the effect lasts
- Therapeutic Window: plasma range that is effective yet not toxic
4. Adverse Effects, Side Effects, and Allergic Reactions
- Side Effects: predictable secondary effects at therapeutic doses
- Adverse Drug Reactions: unintended, harmful reactions at normal doses
- Allergic Reactions: immune‑mediated, from rash to anaphylaxis
- Toxicity: effects from excessive dosing or impaired clearance
5. Drug Efficacy vs. Potency
- Efficacy: maximum effect achievable
- Potency: dose needed for a given effect (lower dose = higher potency); potency does not equal efficacy
6. Therapeutic Index (TI) — Measuring Drug Safety
- Narrow TI: small gap between effective and toxic doses (e.g., digoxin, warfarin, phenytoin, lithium) → requires monitoring
- Wide TI: larger safety margin
NCLEX Tip: Know expected actions and adverse effects, monitor outcomes, educate patients, and link PK with PD (drug levels drive effect intensity and duration).
This article is Part 1 of a three‑part NCLEX pharmacology series.
When you’re ready, continue the journey with
- Part 2 — Drug‑Dosage Calculations & High‑Yield Classifications
- [Part 3 — Medication Safety Essentials & Smart Study Strategies](https://goodnurse.com/article/175/nclex-pharmacology-made-simple-essential-review-of-drugs-calculations-and-key-concepts-part-3