I. Introduction: Why Arrhythmia Mastery Matters
Cardiac arrhythmias—sometimes called dysrhythmias—are disruptions in the heart’s electrical conduction that lead to an abnormal rate or rhythm. On the NCLEX, arrhythmias appear in multiple contexts: interpreting ECG strips, prioritizing interventions, and selecting appropriate medications. Understanding them isn’t just about passing an exam; it’s a life‑saving skill. Quick recognition of lethal rhythms like ventricular fibrillation or torsades de pointes can make the difference between life and death.
This cheat sheet will demystify the most common arrhythmias you’ll encounter on the NCLEX. You’ll learn how to interpret waveforms, identify key characteristics, and recall interventions using mnemonics and memory tricks. Throughout the guide, look for links to deeper resources once they’re published—these placeholders will be updated to live URLs. Use this article along with our cardiac pharmacology review and NCLEX practice quizzes to solidify your understanding.
🎯 Free NCLEX quiz!
See how well you can identify key topics.
II. The Cardiac Conduction System: A Quick Refresher
Before diving into specific arrhythmias, recall the normal electrical pathway of the heart:
- SA node (sinoatrial node) in the right atrium initiates the impulse.
- Impulse spreads through the atria, causing atrial contraction (P‑wave on ECG).
- AV node (atrioventricular node) receives and delays the impulse, allowing ventricles to fill.
- Impulse travels down the Bundle of His, into right and left bundle branches.
- Purkinje fibers distribute the impulse through the ventricles, causing ventricular contraction (QRS complex) and repolarization (T‑wave).
Disruptions in this sequence lead to bradyarrhythmias (slow rhythms), tachyarrhythmias (fast rhythms) or chaotic rhythms like fibrillation. Knowing the normal conduction flow helps you pinpoint where the abnormality originates.
III. Sinus Node Rhythms
A. Normal Sinus Rhythm (NSR)
- Rate: 60–100 beats per minute (bpm).
- Rhythm: Regular; P‑wave precedes each QRS complex.
- PR interval: 0.12–0.20 seconds.
This rhythm indicates the SA node is functioning properly. Variations include sinus bradycardia (<60 bpm) and sinus tachycardia (>100 bpm). Causes of bradycardia include athletic conditioning, vagal stimulation or medications like beta‑blockers; interventions may involve atropine or pacing if symptomatic. Tachycardia often results from fever, pain or hypovolemia; treat the underlying cause and use beta‑blockers or calcium channel blockers if necessary.
B. Sinus Arrhythmia
- Rate: 60–100 bpm.
- Rhythm: Irregular, often correlating with breathing (inspiration speeds up, expiration slows down).
- Interventions: Typically benign; no treatment required unless symptomatic.
IV. Atrial Rhythms
A. Atrial Fibrillation (AF)
- Rhythm: Irregularly irregular; no discernible P‑waves.
- Rate: Atrial rate can be 300–600 bpm; ventricular rate varies.
- Clinical significance: Loss of atrial kick reduces cardiac output; high risk of thrombus formation and stroke.
- Interventions: Rate control with beta‑blockers, calcium channel blockers or digoxin; rhythm control with antiarrhythmic drugs or cardioversion; anticoagulation to prevent stroke.
- Mnemonic: “A‑fib is a quivering jelly”—think of atria shaking like jelly without effective contraction.
B. Atrial Flutter
- Rhythm: Regular or regularly irregular; “sawtooth” flutter waves instead of P‑waves.
- Atrial rate: 250–350 bpm.
- Clinical significance: Can reduce cardiac output and cause palpitations; may lead to thrombus formation.
- Interventions: Rate control similar to AF, anticoagulation, and possible ablation.
- Mnemonic: “Flutter has a pattern”—those sawtooth waves create a rhythmic pattern.
C. Supraventricular Tachycardia (SVT)
- Rate: 150–250 bpm.
- Rhythm: Regular, narrow QRS complexes.
- Symptoms: Palpitations, dizziness, shortness of breath; may cause hypotension.
- Interventions: Vagal maneuvers (bearing down, carotid massage), adenosine IV push (slows AV conduction), beta‑blockers, synchronized cardioversion if unstable.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
V. Junctional and AV Node Rhythms
A. Premature Junctional Contractions (PJCs)
- Rhythm: Underlying rhythm interrupted by early QRS complexes with inverted or absent P‑waves.
- Cause: Enhanced automaticity of the AV junction; often benign.
- Interventions: Usually none; treat underlying causes like caffeine or stress.
B. Junctional Escape Rhythm
- Rate: 40–60 bpm.
- Rhythm: Regular; P‑waves absent, inverted or follow the QRS.
- Interventions: If symptomatic bradycardia, administer atropine or consider pacing.
C. Accelerated Junctional Rhythm / Junctional Tachycardia
- Rate: Accelerated: 60–100 bpm; Junctional tachycardia: >100 bpm.
- Interventions: Similar to SVT—vagal maneuvers and AV nodal blocking agents.
VI. Ventricular Rhythms
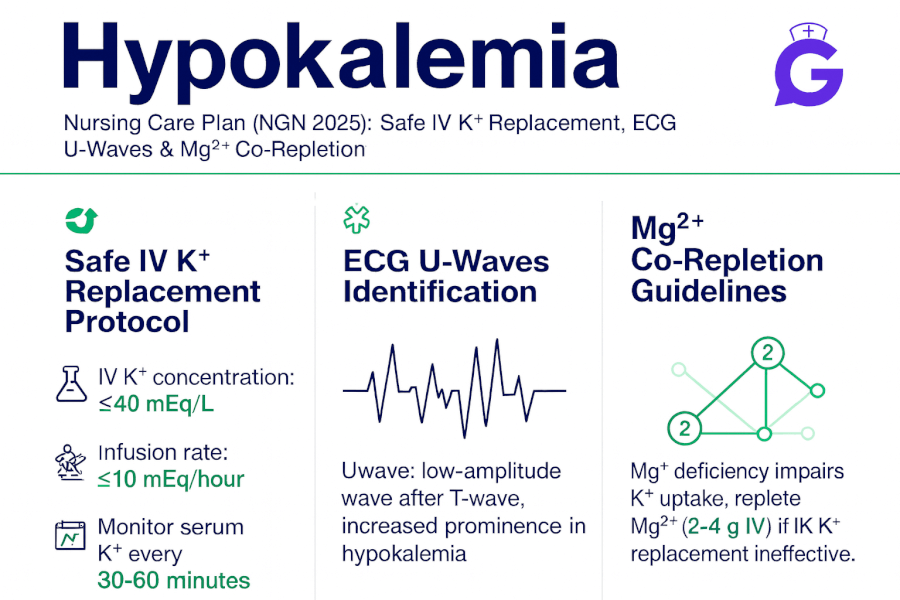
A. Premature Ventricular Contractions (PVCs)
- Features: Early, wide QRS complexes not preceded by P‑waves; followed by a compensatory pause.
- Causes: Hypoxia, electrolyte imbalances (especially low potassium or magnesium), stimulants like caffeine.
- Interventions: Treat the underlying cause; if frequent or symptomatic, consider antiarrhythmics (e.g., amiodarone) and correct electrolytes.
- Mnemonic: “Lidocaine for lots of PVCs”—though not first‑line anymore, it helps remember the association.
B. Ventricular Tachycardia (VT)
- Rate: 100–250 bpm.
- Rhythm: Regular; wide QRS complexes; may be monomorphic or polymorphic (torsades de pointes).
- Symptoms: Palpitations, dizziness, hypotension, potential progression to V‑fib.
- Interventions: If pulse present and patient stable, administer antiarrhythmics (amiodarone or procainamide) or perform synchronized cardioversion. If no pulse, treat as pulseless VT with immediate CPR and defibrillation. For torsades de pointes, give intravenous magnesium.
C. Ventricular Fibrillation (VF)
- Rhythm: Chaotic, irregular waves with no identifiable QRS complexes; no cardiac output.
- Interventions: Immediate CPR and defibrillation. Administer epinephrine and amiodarone per advanced cardiac life support (ACLS) guidelines. This rhythm is fatal if not corrected promptly.
D. Asystole
- Rhythm: Flat line; no electrical activity.
- Interventions: CPR and epinephrine; confirm asystole on more than one lead; check patient leads; do not shock, as there is no electrical activity to reset.
VII. Heart Blocks: First to Third Degree
A. First‑Degree AV Block
- Features: Prolonged PR interval (>0.20 seconds) but constant; every P‑wave followed by a QRS.
- Clinical significance: Usually benign; may be caused by medications (digoxin, beta‑blockers) or ischemia.
- Interventions: Monitor; treat underlying cause.
B. Second‑Degree AV Block Type I (Mobitz I/Wenckebach)
- Features: Progressive prolongation of the PR interval until a QRS is dropped.
- Interventions: Usually asymptomatic; monitor. If symptomatic bradycardia, atropine may be used.
C. Second‑Degree AV Block Type II (Mobitz II)
- Features: Fixed PR interval with intermittent dropped QRS complexes.
- Clinical significance: More serious; can progress to third‑degree block.
- Interventions: Often requires pacing; treat symptomatic bradycardia promptly.
D. Third‑Degree (Complete) AV Block
- Features: No relation between P‑waves and QRS complexes; atria and ventricles beat independently.
- Symptoms: Severe bradycardia, dizziness, syncope, hypotension.
- Interventions: Immediate pacing (temporary or permanent) and supportive care.
VIII. Nursing Priorities and Interventions
- Assess hemodynamic stability: Always assess your patient—level of consciousness, blood pressure, oxygen saturation, chest pain—before treating an arrhythmia.
- Ensure airway, breathing and circulation (ABCs): For unstable patients, initiate CPR or call for help immediately.
- Monitor ECG continuously: Identify rhythm changes early. Document onset, pattern and patient symptoms.
- Administer medications safely: Know indications, contraindications and dosages of antiarrhythmics, beta‑blockers, calcium channel blockers and anticoagulants.
- Prepare for cardioversion or defibrillation: For unstable tachyarrhythmias or lethal rhythms. Know the difference between synchronized cardioversion (for rhythms with a pulse) and unsynchronized defibrillation (for pulseless VT/VF).
- Provide patient education: Teach clients about medication adherence, lifestyle modifications (reducing caffeine and alcohol, quitting smoking), and when to seek medical attention.
- Collaborate with the interdisciplinary team: Work with cardiologists, pharmacists and respiratory therapists to optimize care.
IX. Quick Reference Mnemonics for Arrhythmias
- “If QRS is wide, think ventricular in stride.” Wide QRS complexes suggest ventricular origin (e.g., VT, PVCs).
- “Irregularly irregular equals A‑fib.” Atrial fibrillation’s hallmark is a chaotic, irregular rhythm.
- “Sawtooth flutter is better.” Atrial flutter shows sawtooth waves.
- “For SVT, try to VAGAL and give ADEN.” Vagal maneuvers and adenosine treat supraventricular tachycardia.
- “Dead rhythms (VF/VT without pulse) need DEFIB.” Defibrillate pulseless VT and VF; do not defibrillate asystole.
X. Final Thoughts and Further Resources
Mastering arrhythmias requires practice—studying ECG strips, recognizing patterns and understanding interventions. Use this cheat sheet as a quick reference while you prepare for the NCLEX and clinical practice. When the detailed article goes live, the placeholder link above will be replaced with a comprehensive arrhythmia guide that includes practice questions and downloadable rhythm strips.
Continue building your cardiac knowledge by exploring these GoodNurse articles:
- NCLEX Cardiovascular Drugs In‑Depth: Learn about ACE inhibitors, beta‑blockers, calcium channel blockers and nitrates.
- NCLEX Study Tips That Actually Work in 2025: Develop a personalized study plan with active learning strategies.
- Pediatric Nursing Growth & Development Milestones: Brush up on developmental milestones for the pediatric portion of the exam.
By understanding how to recognize and respond to arrhythmias, you’ll enhance patient safety and boost your confidence on the NCLEX. Keep practicing, review this cheat sheet regularly and pair it with our practice quizzes to test your rhythm interpretation skills.