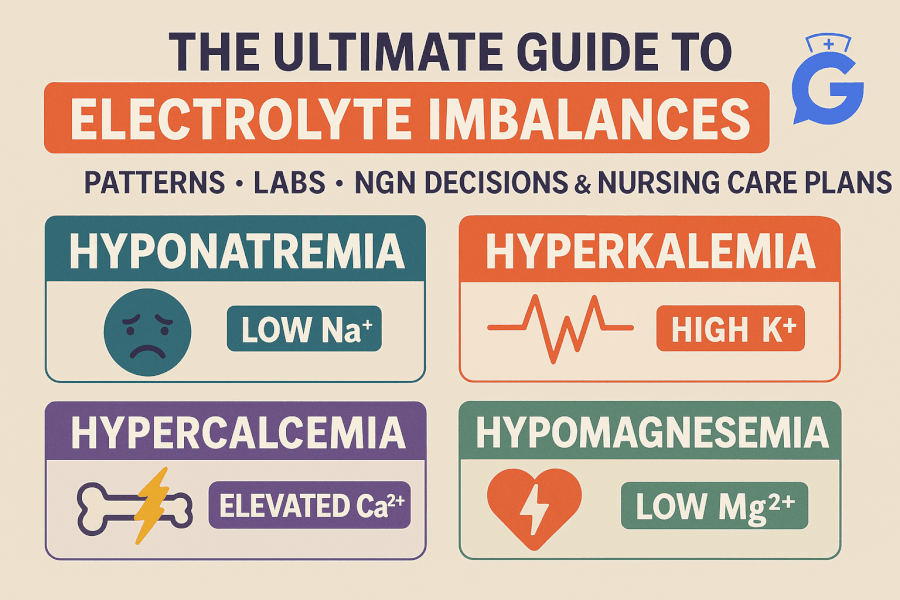
Electrolyte questions on the Next Gen NCLEX reward pattern recognition and prioritized action. This pillar is your hub: frameworks you can reuse at the bedside, master tables that compress the chaos into a few decisions, and deep links to our detailed care plans and study hubs.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Keep these study hubs open in another tab for quick lookups:
• Electrolyte Imbalances Made Easy (Mnemonics)
• Electrolytes Cheat Sheet
• ABG Interpretation—15 Cases
Table of Contents
- How to Think About Electrolytes (Reusable Frameworks)
- Master Pattern Tables (Symptoms → Labs → First Safe Steps)
- Sodium: Volume, Tonicity, and the Brain
- Potassium: ECG-First, Stabilize–Shift–Remove
- Calcium: Tetany vs Calcifications
- Magnesium: The Quiet Driver
- Phosphate: CKD-MBD, Ca×P Reality, Binder Timing
- Acid–Base Crossovers (ABG Shortcuts)
- Replacement & Correction Quick-Refs
- NGN Micro-Cases (20 practice vignettes)
- Myths vs Facts
- OTC Pitfalls & Safety Alerts
- FAQ (25+ PAA-style questions)
- References
How to Think About Electrolytes (Reusable Frameworks)
1) Life over numbers
- If unstable (airway, seizure, malignant arrhythmia), treat now, even before the full lab panel is back.
2) The four playbooks you’ll use most
- Potassium (↑K⁺): Stabilize → Shift → Remove → Prevent. Start with membrane stabilization when ECG is dangerous. See Hyperkalemia.
- Sodium (↑/↓ Na⁺): Rate-limited correction and careful volume assessment. See Hypernatremia.
- Calcium/Magnesium: ECG + neuro first; antagonize toxicity (IV Ca for Mg toxicity), or replace deficits. Co-replete Mg²⁺ if K⁺ won’t budge. See Hypomagnesemia.
- Phosphate (PO₄³⁻): Trend-then-treat; binders with bites (timed with meals), and optimize dialysis in CKD-MBD. See Hyperphosphatemia and Hypophosphatemia.
3) Trend + teach-back
- Numbers bounce; document the direction and verify patient understanding (dietary additives, laxatives, diuretics, insulin, dialysis adherence).
Master Pattern Tables (Symptoms → Labs → First Safe Steps)
| Symptom Cluster | Probable Culprit | Focused Labs/Tests | First Safe Steps | Go Deeper |
|---|---|---|---|---|
| Seizure/tetany, perioral tingling | ↓Ca²⁺ or ↑PO₄³⁻ | Ionized Ca²⁺, PO₄³⁻, PTH, Vit D | Seizure precautions; check phosphate; treat underlying | Hypocalcemia • Hyperphosphatemia |
| Peaked T waves, weakness | ↑K⁺ | BMP, ECG | Calcium (stabilize), insulin/glucose (shift), removal | Hyperkalemia |
| U waves, ileus, dig sensitivity | ↓K⁺ | BMP, Mg²⁺ | Replete K⁺; check Mg²⁺ | Hypokalemia |
| Thirst, confusion, lethargy | Hypernatremia | Serum/urine osms, volume status | Rate-limited free water correction | Hypernatremia |
| Torsades, alcohol use, diuretics | ↓Mg²⁺ | Mg²⁺, K⁺, ECG | IV Mg²⁺; co-replete K⁺ | Hypomagnesemia |
| Loss of DTRs, respiratory depression (OB infusion) | ↑Mg²⁺ | Mg²⁺, ECG | Stop Mg²⁺; IV calcium; support ventilation | Hypermagnesemia |
| Pruritus, bone pain, CKD | CKD-MBD (↑PO₄³⁻) | PO₄³⁻, Ca²⁺ (ionized), PTH | Diet + binders with meals; dialysis plan | Hyperphosphatemia |
Sodium: Volume, Tonicity, and the Brain
Workflow (hypernatremia-focused)
- Check volume (dry mucosa, orthostasis? DI vs dehydration?).
- Calculate free water deficit conceptually; rate-limit correction to protect the brain.
- Reassess sodium at safe intervals; track I/O and mental status.
Deep dive: Hypernatremia Care Plan
Micro-quiz: When correcting chronic hypernatremia, is faster always better? → No; over-rapid drops risk cerebral edema. (See care plan above.)
Potassium: ECG-First, Stabilize–Shift–Remove
Algorithm you can recite
- Stabilize: IV calcium for life-threatening ECG.
- Shift: insulin/glucose; consider β-agonist; bicarbonate if acidemic.
- Remove: resins, diuretics, dialysis.
- Prevent: review meds/renal function, add GI plan.
Full protocol: Hyperkalemia.
If K⁺ repletion won’t “stick,” think magnesium: Hypomagnesemia.
Calcium: Tetany vs Calcifications
Pearls that show up on NGN
- Corrected vs ionized Ca²⁺: When albumin is abnormal or patient symptomatic, ionized Ca²⁺ tells the real story.
- Massive transfusions: citrate can chelate calcium → acute hypocalcemia (watch ECG).
- High calcium differentials: primary HPT vs malignancy (PTH-driven vs PTH-independent).
Go deeper:
Magnesium: The Quiet Driver
- Low Mg²⁺ → torsades risk; High Mg²⁺ → loss of DTRs, respiratory depression (e.g., OB therapy).
- Antagonize toxicity: IV calcium; support ventilation.
- Co-repletion rule: replace Mg²⁺ alongside K⁺ to make K⁺ repletion effective.
Read: Hypomagnesemia • Hypermagnesemia
Phosphate: CKD-MBD, Ca×P Reality, Binder Timing
- CKD → phosphate retention → ↑FGF23/↓calcitriol → secondary hyperparathyroidism → bone & vascular complications.
- Binders with bites: sevelamer/lanthanum/ferric citrate with meals/snacks; restrict calcium-based binders when hypercalcemia/calcification risk exists.
- Avoid sodium phosphate OTCs in CKD unless specifically directed.
Read both sides:
Acid–Base Crossovers (ABG Shortcuts)
- Check anion gap when K⁺ is off and the story suggests DKA/renal failure.
- Use Winters formula logic to sanity-check compensation.
- Practice here: ABG Interpretation—15 Cases
Replacement & Correction Quick-Refs
Safety note: Always follow your facility’s protocols. These bullets help you reason for exams and pre-rounds; dosing is intentionally generalized for NCLEX thinking, not bedside orders.
- Sodium: Rate-limit correction; frequent labs and neuro checks. (Hypernatremia)
- Potassium: IV vs PO depends on severity/ECG/route tolerance; fix Mg²⁺ if K⁺ won’t correct.
- Magnesium: Torsades or severe symptoms → IV Mg²⁺ first; monitor DTRs and respiratory status.
- Calcium: Symptomatic hypocalcemia → IV calcium with ECG monitoring; interpret alongside phosphate and albumin/ionized Ca²⁺.
- Phosphate: Severe/symptomatic low → IV phosphate carefully (watch Ca²⁺/Mg²⁺); high in CKD → diet + binders with meals; optimize dialysis.
NGN Micro-Cases (20 practice vignettes)
Use the links under each answer for deeper study. Mix of matrix/grid, bow-tie, and case stems.
- Matrix/Grid — HyperK rapid fire
A 58-year-old with AKI has K⁺ 6.8, peaked T waves. Choose all that apply (initial actions):
- Start sevelamer
- Give IV calcium
- Give insulin + dextrose
- Schedule outpatient nephrology next week
Rationale → Stabilize–Shift–Remove. See Hyperkalemia.
-
Bow-Tie — HyperNa (DI vs dehydration)
Center: 24-h polyuria, serum Na⁺ 154, urine osms low.
Left (Causes): central DI; nephrogenic DI.
Right (Actions): desmopressin trial; free water replacement; monitor sodium correction rate.
Study → Hypernatremia. -
Case Stem — HypoMg with refractory hypokalemia
K⁺ 3.0 despite IV/PO replacement; Mg²⁺ 1.3; U waves on ECG.
Best next step: Replace Mg²⁺ first or concurrently.
Study → Hypomagnesemia. -
Matrix/Grid — Hypocalcemia after transfusions
Massive transfusion, paresthesias, prolonged QT.
- Check ionized Ca²⁺
- Administer IV calcium if symptomatic
- Give phosphate enema
Study → Hypocalcemia.
-
Case Stem — CKD-MBD pruritus
HD patient, PO₄³⁻ 6.1, Ca²⁺ 8.3, PTH ↑; heavy processed foods.
Two first actions: diet counseling on phos- additives; start sevelamer with meals per order.
Study → Hyperphosphatemia. -
Bow-Tie — TLS electrolyte storm
Causes: tumor lysis → ↑K⁺, ↑PO₄³⁻, ↓Ca²⁺.
Actions: cardiac monitoring, cautious calcium only for symptomatic hypocalcemia, consider dialysis if severe.
Read → (see phosphate/care plan and ABG hub). -
Matrix/Grid — HyperMg from OB infusion
- Stop Mg²⁺ infusion
- IV calcium to antagonize effects
- Support ventilation/respirations
Study → Hypermagnesemia.
-
Case Stem — Calcium stone history
Recurrent stones; Ca-phosphate type suspected. Teach hydration and evaluate contributing meds/diet.
Study → Calcium Stones. -
Matrix/Grid — Hypercalcemia of malignancy
- Aggressive isotonic fluids (if not contraindicated)
- Calcitonin for rapid but short-term drop
- Antiresorptive therapy per oncology
Study → Hypercalcemia of Malignancy.
-
Case Stem — Primary HPT
Elevated Ca²⁺, elevated PTH; bone pain. Pre-op teaching and hydration priority.
Study → Primary Hyperparathyroidism. -
Matrix/Grid — HypoK on digoxin
- Replete K⁺ cautiously
- Monitor ECG closely
- Give sodium phosphate enema
Study → Hypokalemia.
- Case Stem — Refeeding risk
Malnourished; PO₄³⁻ dropping after nutrition started; respiratory weakness.
Action: controlled refeeding; IV/PO phosphate per protocol; monitor Mg²⁺/K⁺.
Study → Hypophosphatemia.
13–20) Create additional variations mixing Na⁺/K⁺/Ca²⁺/Mg²⁺/PO₄³⁻ with ABG clues and dialysis scenarios; link to the relevant care plans above.
Myths vs Facts
-
Myth: “Always target Ca×P <55.”
Fact: Know the history; modern guidance emphasizes individual Ca²⁺ and PO₄³⁻ trends in CKD-MBD decisions. -
Myth: “IV calcium fixes every prolonged QT.”
Fact: Avoid indiscriminate IV calcium in severe hyperphosphatemia/TLS—risk of Ca-phosphate precipitation. Give calcium for symptomatic hypocalcemia while you lower phosphate. -
Myth: “If K⁺ is low, just give more K⁺.”
Fact: If Mg²⁺ is low, K⁺ won’t correct; co-replete.
OTC Pitfalls & Safety Alerts
- Sodium phosphate enemas/oral purgatives: In CKD, misuse or exceeding labeled doses can cause dangerous electrolyte shifts—avoid unless specifically directed.
- “Phos-” additives in processed foods: Highly absorbable and a major driver of phosphate load. Teach label reading.
FAQ (25+ PAA-style questions)
-
What order should I correct multiple derangements in?
Stabilize life-threatening issues (arrhythmias/seizure), then correct the driver (DKA, dehydration), while rate-limiting sodium changes and co-repleting Mg²⁺ with K⁺. -
When should I use ionized calcium instead of total?
When albumin is abnormal, the patient is symptomatic, or the clinical picture doesn’t match total Ca²⁺. -
How fast can I correct hypernatremia?
Use conservative, protocol-based rates to avoid cerebral edema; see Hypernatremia Care Plan. -
Which binders are calcium-free?
Sevelamer, lanthanum, ferric citrate—preferred when hypercalcemia or calcification risk exists. See Hyperphosphatemia. -
When is dialysis indicated for electrolytes?
Refractory ↑K⁺ or ↑PO₄³⁻ despite medical therapy; emergent settings like TLS/AKI with life-threatening profiles. -
Does hypomagnesemia cause arrhythmias?
Yes—torsades risk; treat with IV Mg²⁺. See Hypomagnesemia. -
Do I still calculate Ca×P?
Know it for context, but decisions rely on Ca²⁺ & PO₄³⁻ values/trends, CKD stage, and calcification risk. -
What ECG changes match K⁺ extremes?
↑K⁺: peaked T → sine wave; ↓K⁺: U waves. See 229 and 230. -
Transfusion-related hypocalcemia—what to do first?
Check ionized Ca²⁺ and give IV calcium if symptomatic; monitor ECG. See 224. -
Which foods secretly spike phosphate?
Processed meats, colas, shelf-stable products with “phos-” additives—teach label reading.
11–25) Add more from your cohort’s questions during class and clinicals; link to the appropriate care plans above.
References
- KDIGO. Clinical Practice Guideline Update for CKD–MBD (2017). https://kdigo.org/guidelines/ckd-mbd/
- NIDDK (NIH). Mineral & Bone Disorder in Chronic Kidney Disease. https://www.niddk.nih.gov/health-information/kidney-disease/mineral-bone-disorder
- U.S. FDA. Drug Safety Communication: Risks from over-the-counter sodium phosphate products. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-over-the-counter-sodium-phosphate-products
- NIH Office of Dietary Supplements. Magnesium—Health Professional Fact Sheet. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- NIH Office of Dietary Supplements. Potassium—Health Professional Fact Sheet. https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional/
- MedlinePlus (NIH). Electrolytes. https://medlineplus.gov/electrolytes.html