When a patient has tremors, PVCs, and “K⁺ just won’t budge,” think magnesium. In clinicals I’ve watched students chase potassium for hours—until someone checks Mg²⁺. This NGN-ready guide gives you a calm, practical plan: concise pathophysiology, prioritized nursing diagnoses with SMART outcomes, and interventions with rationales (telemetry safety, IV vs PO replacement, and how Mg²⁺ ties to K⁺ and Ca²⁺). Use it for pre-conference, simulation, or documenting care at the bedside.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Pathophysiology of Hypomagnesemia
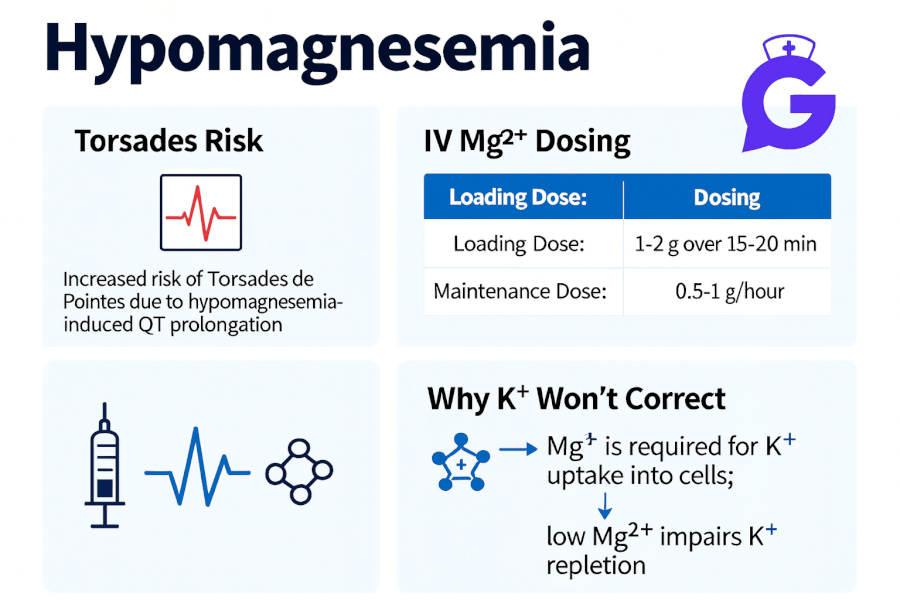
Hypomagnesemia (institution ranges vary; often < 1.7–1.8 mg/dL) increases neuromuscular excitability and destabilizes myocardial conduction. Magnesium modulates calcium influx and potassium transport; when Mg²⁺ is low, patients are prone to ventricular ectopy and torsades de pointes (polymorphic VT), and potassium becomes refractory to repletion. Common causes:
- GI losses/malabsorption: diarrhea, fistulas, IBD, celiac disease, post-Whipple, chronic PPI use
- Renal losses: loop/thiazide diuretics, aminoglycosides, amphotericin B, cisplatin, tacrolimus, poorly controlled diabetes
- Inadequate intake/alcohol use disorder and refeeding
- Shifts: pancreatitis (saponification), hyperaldosteronism
Clinical clues: tremor, muscle cramps, positive Chvostek/Trousseau (via linked hypocalcemia), nystagmus, seizures, and ECG changes (prolonged QT/QTc, widened QRS, ventricular ectopy). Management priorities: 1) cardiac safety (telemetry for moderate–severe or symptomatic cases), 2) replace magnesium (PO for mild; IV for moderate–severe or symptomatic), 3) co-replete potassium if low, and 4) address the cause (diuretics, PPIs, alcohol, diarrhea).
Fast Assessment & Monitoring (bedside)
- Confirm hypomagnesemia: check Mg²⁺ (and ionized Ca²⁺, K⁺, phosphate).
- Telemetry/ECG: assess for QT prolongation, ectopy, torsades risk.
- Look for drivers: diuretics, PPI/chemo, diarrhea, alcohol use, malnutrition.
- Repletion route: PO for mild/asymptomatic and intact GI; IV for symptomatic, arrhythmias, seizures, or malabsorption.
- Trend labs: recheck Mg²⁺ (and K⁺) after replacement per facility protocol; monitor DTRs and sedation with IV therapy.
Reinforce your clinical judgment with: Hyperkalemia Care Plan, Hypokalemia Care Plan, and Hypernatremia Care Plan—plus calcium cluster pages (/223, /224, /226, /227, /228), and study helpers /184, /203, /201, /195.
Nursing Care Plans for Hypomagnesemia
Individualize goals and dosing to your facility protocols and provider orders. These NGN-style plans prioritize arrhythmia prevention and effective repletion.
Nursing Diagnosis: Risk for Decreased Cardiac Output (dysrhythmias including torsades)
| Category | Details |
|---|---|
| Related to | Prolonged repolarization and increased ventricular irritability from low Mg²⁺ |
| As evidenced by | (Risk state) QT/QTc prolongation, PVCs, ventricular tachyarrhythmias; concurrent hypokalemia |
| Desired Outcomes | Maintains stable rhythm; QTc trends toward baseline; no VT/torsades; Mg²⁺ reaches provider target within 6–24 h. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Place on continuous cardiac monitoring; obtain baseline and follow-up ECGs. | Detects torsades and other ventricular rhythms early; documents response to repletion. |
| Administer IV magnesium sulfate per protocol for symptomatic or significant hypomagnesemia; keep calcium gluconate available if high-dose Mg²⁺ depresses respiration. | IV Mg²⁺ stabilizes myocardium and shortens QT; monitoring prevents over-sedation and respiratory compromise. |
| Co-replete potassium if low; reassess K⁺/Mg²⁺ after each replacement cycle. | Corrects refractory hypokalemia driven by Mg²⁺ deficiency. |
Nursing Diagnosis: Risk for Electrolyte Imbalance (ongoing losses/malabsorption)
| Category | Details |
|---|---|
| Related to | Diuretic therapy, diarrhea/malabsorption, alcohol use disorder, chemotherapy, PPIs |
| As evidenced by | Recurrent low Mg²⁺, low K⁺, low Ca²⁺; poor intake; GI losses; high urine Mg²⁺ if renal wasting |
| Desired Outcomes | Mg²⁺ sustained in target range; reduced need for repeat repletion; cause addressed or mitigated. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Review meds (loop/thiazide diuretics, PPIs, nephrotoxic agents); collaborate on adjustments or substitutes. | Reduces renal/GI magnesium wasting. |
| Initiate PO magnesium for mild/asymptomatic cases if GI tract is functional; provide GI side-effect counseling. | Builds stores with lower toxicity risk; mitigates diarrhea/loose stools that can worsen losses. |
| Coordinate nutrition support (dietary Mg sources) and alcohol cessation resources as appropriate. | Addresses intake deficits and lifestyle drivers. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Deficient Knowledge (replacement safety & recurrence prevention)
| Category | Details |
|---|---|
| Related to | Unfamiliarity with IV/PO Mg²⁺ dosing, monitoring, and interactions; misunderstanding of K⁺/Ca²⁺ links |
| As evidenced by | Questions about infusion rates, diarrhea management, binder interactions, and lab follow-up |
| Desired Outcomes | Patient/family teach back home plan, med timing, diet sources, and return precautions before discharge. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach IV safety: use infusion pump and continuous monitoring as indicated; follow facility protocol for rate/monitoring. | Prevents hypotension, flushing, and respiratory depression from rapid infusions. |
| Review common interactions (e.g., Mg²⁺ with certain antibiotics) and GI tips (take PO Mg with food; split dosing to limit diarrhea). | Improves adherence and reduces side effects that can worsen losses. |
| Explain the Mg²⁺–K⁺–Ca²⁺ connection; set expectations that K⁺ may not normalize until Mg²⁺ is corrected. | Aligns patient and team on sequencing and goals. |
Frequently Asked Questions (FAQ)
Why won’t potassium correct if magnesium is low?
Mg²⁺ deficiency increases renal K⁺ wasting and impairs cellular uptake, making hypokalemia refractory. Replete magnesium first (or concurrently) so K⁺ will stabilize.
When should magnesium be given IV vs PO?
Use IV for symptomatic patients, significant ECG changes/arrhythmias, seizures, or malabsorption; PO for mild/asymptomatic cases with intact GI and reliable follow-up. Always follow provider orders and facility protocols.
What are signs of magnesium toxicity?
Flushing, hypotension, diminished deep tendon reflexes, somnolence, and in severe cases respiratory depression or heart block—monitor vitals and DTRs during IV therapy and keep calcium available per protocol.
Which foods have magnesium?
Nuts, seeds, legumes, whole grains, leafy greens, and fortified cereals are rich in Mg²⁺ (see NIH ODS fact sheet below).
Further Reading
- Hyperkalemia Nursing Care Plan
- Hypokalemia Nursing Care Plan
- Hypernatremia Nursing Care Plan
- Hypercalcemia Nursing Care Plan
- Hypocalcemia Nursing Care Plan
- Primary Hyperparathyroidism Nursing Care Plan
- Hypercalcemia of Malignancy Nursing Care Plan
- Calcium Kidney Stones (Nephrolithiasis) Care Plan
- Electrolyte Imbalances Made Easy
- Electrolytes Cheat Sheet
- ABG Interpretation: 15 Practice Cases
- NGN Med-Surg Case Studies