Safe Rounding Rules for NCLEX (2025): Tablets, Liquids, IV mL/hr & gtt/min, and Syringe Pumps If we were in skills lab together, I’d start with a confession: most calculation “errors” I see aren’t math—they’re rounding. A half tablet trimmed like a pizza slice, a liquid dose rounded to a household teaspoon, an IV rate set to a pretty number. On a peds unit or during NCLEX, that sloppiness turns into risk fast.
My goal in this guide is simple: give you a professor-tested rounding playbook you can apply in seconds—tablets, oral liquids, IV mL/hr, gtt/min, and syringe pumps—plus where pediatric micro-dosing breaks the usual rules. I’ll also point to authoritative safety guidance as we go, like the Institute for Safe Medication Practices’ work on liquid-measurement errors (ISMP) and university dosage-calc handouts (Upstate.edu, Bergen.edu). Keep this in your NCLEX binder next to dosage math refreshers like our peds mg/kg guide: Pediatric Dosage Calculations (2025).
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- Why Rounding Matters: Safety Principles & Official Guidance
- Route-by-Route Rules: Tablets, Liquids, IV mL/hr, gtt/min, Syringe Pumps
- Practice: 15 Quick Rounding Items with Professor’s Rationale
- FAQs
- Key Takeaways
- Further Reading
Why Rounding Matters: Safety Principles & Official Guidance
NCLEX and bedside safety reward consistency. When your units cancel cleanly and your rounding aligns with policy, the correct answer is often the only answer that “looks right.” Here’s the safety frame I teach:
- Use metric devices—never kitchen spoons. ISMP and the AAP warn that household spoons create large errors for oral liquids; use an oral syringe and round appropriately for the smallest graduation (ISMP liquid-med safety; AAP: Using Liquid Medicines).
- Match rounding to the delivery device. Syringe graduations (0.1 mL vs 0.01 mL), pump settings (whole mL/hr vs decimal), and drip sets (60 gtt/mL micro vs 10–20 macro) dictate what’s reasonable (Bergen.edu).
- Pediatrics ≠ adults. Small bodies + narrow therapeutic ranges mean micro-rounding is often required; some doses cap at maximum daily dose (MDD) even if your math says otherwise (AAP dosing tables for acetaminophen/ibuprofen: AAP acetaminophen; AAP ibuprofen).
- Gravity drips round to whole drops. Because you can’t run a fraction of a drop, gtt/min answers are whole numbers. University skill sheets reinforce this convention (Upstate.edu).
Professor’s note: My 5-second check: “Does my final number match the device?” If I calculated **0.07 mL** for a med drawn with a 1 mL syringe marked every **0.1 mL**, I know I either need a different syringe or I misread the concentration.
For a broader infusion refresher before you dive into rounding practice, skim our concise setup guide: IV Drip Rates & Infusions. And if you’d like an older staple for physiology context during titrations, our ABG pattern primer pairs well here: ABG Interpretation (2025).
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Route-by-Route Rules: Tablets, Liquids, IV mL/hr, gtt/min, Syringe Pumps
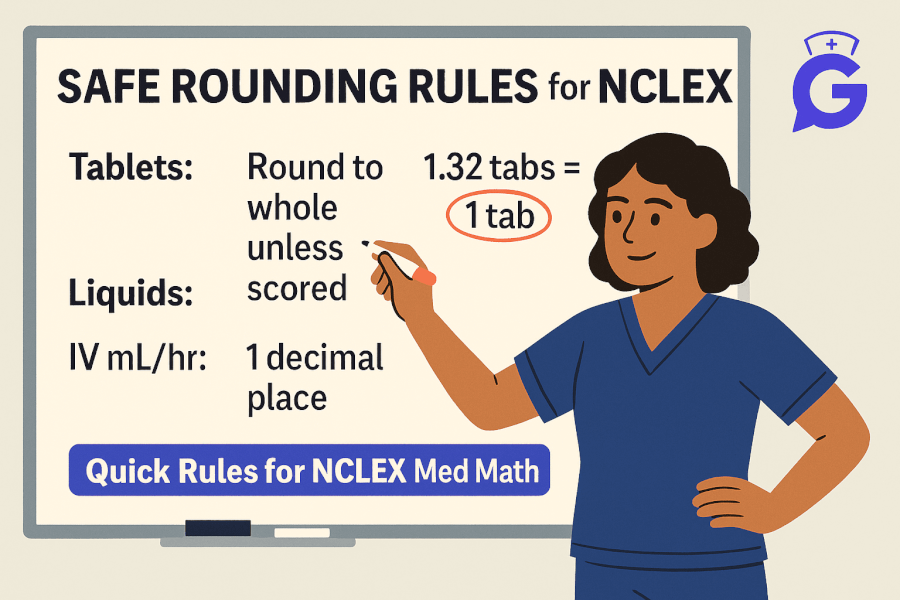
Tablets (scored vs. unscored; modified release)
- Scored tablets may be split according to markings; round to the nearest ½ tablet (or ¼ if scored accordingly).
- Do not split unscored or modified-release forms (SR/ER/XL/EC). If your math yields 1.3 tablets of an ER med, the correct action is to find an alternative strength, not to round.
- NCLEX convention: If options are in tablets and a scored split is safe, round to the nearest scored fraction.
Anecdote from precepting: I’ve watched students “shave” tablets to make 0.8 into “almost one.” That’s not rounding—that’s altering the dose and the release profile. On test day, choose the fraction that the tablet can safely deliver.
Oral liquids (syringes & cups)
- Use oral syringes for small volumes; round to the nearest 0.1 mL unless your device or policy supports 0.01 mL (common in NICU/peds).
- Medication cups are reasonable ≥5 mL; still, many units prefer syringes for accuracy.
- Avoid teaspoon/tablespoon conversions; FDA and AAP promote metric-only dosing devices to reduce errors (FDA; AAP).
IV pump rates (mL/hr)
- Unless otherwise specified, set pumps to whole mL/hr.
- When decimal precision is ordered (e.g., 0.5 mL/hr for a vasoactive or neonatal med), use a syringe pump capable of that resolution.
- If your math yields 39.6 mL/hr, standard practice is 40 mL/hr unless the order states “no rounding.” Verify policy.
Gravity drips (gtt/min)
- Calculate mL/hr first, then convert:
[ \text{gtt/min}=\frac{\text{mL/hr} \times \text{drop factor (gtt/mL)}}{60} ] - Round to a whole drop. With a 60 gtt/mL (microdrip), 20 mL/hr = (20×60/60=20) gtt/min—already whole.
- With macrodrips (10–20 gtt/mL), numbers often land between integers—round to the nearest whole gtt/min (Bergen.edu).
Syringe pumps (NICU/Peds micro-dosing)
- Follow unit policy; many require rounding to the nearest 0.01 mL for tiny volumes.
- Extremely small volumes may require dilution to achieve device accuracy; your calculation then uses the final concentration.
- Link back to mg/kg logic and MDD caps before final rounding—see our step-by-step peds practice: Pediatric Dosage Calculations.
Professor’s note: Let the **device** and **policy** decide the decimal place. If your result can’t be set on the device, adjust concentration (with an order) or select a different delivery route—not a “creative” rounding shortcut.
Keep growing your NGN pattern recognition with older, still-evergreen practice on item formats that demand precise calculations: NGN Matrix/Grid Items (2025) and our early deep-dive on AI study workflows for accuracy under time pressure: Best AI Apps for Nursing Students (2025).
Practice: 15 Quick Rounding Items with Professor’s Rationale
Assume typical rounding unless stated; follow local policy on your unit/school.
-
Tablet: Order 375 mg; available 250 mg scored tablets.
Calculation: 1.5 tablets → Give 1½ tablets (scored permits halves). -
Tablet (ER): Order 37.5 mg ER; available 25 mg ER tablets (unscored).
Do not split ER. Call for alternative strength to reach 37.5 mg safely. -
Oral liquid: Need 4.73 mL using 1 mL oral syringe marked every 0.1 mL.
4.7 mL (nearest 0.1 mL). -
Oral liquid (NICU): Need 0.086 mL; syringe supports 0.01 mL.
0.09 mL (nearest 0.01 mL) or dilute per policy to improve accuracy. -
IV pump: Infuse 100 mL over 2.5 hr.
40 mL/hr exactly → 40 mL/hr. -
IV pump: Rate calc = 39.6 mL/hr; no special precision ordered.
40 mL/hr (round to whole mL/hr). -
Gravity drip: 100 mL over 30 min; 15 gtt/mL set.
mL/hr = 200 → gtt/min = (200×15/60=50) → 50 gtt/min (whole). -
Gravity drip: Calc = 22.4 gtt/min; 10 gtt/mL set.
22 gtt/min (nearest whole drop). -
Syringe pump (peds): 0.724 mL/hr with 0.01 mL/hr resolution.
0.72 mL/hr (nearest 0.01). -
Syringe pump (decimal restriction): 0.734 mL/hr; device steps of 0.05 mL/hr only.
0.75 mL/hr if policy permits rounding up (or adjust concentration to meet the order exactly). -
Peds acetaminophen: 8.72 mL; oral syringe to 0.1 mL.
8.7 mL; confirm MDD vs age/weight (see AAP tables linked above). -
Insulin infusion rate display: Calc 2.84 mL/hr; pump shows one decimal place only.
2.8 mL/hr unless protocol requires exact; some DKA pathways specify acceptable rounding—defer to policy. -
Heparin units/hr to mL/hr: Result 2.12 mL/hr; pump allows two decimals.
2.1 mL/hr (nearest 0.1) unless protocol dictates two decimals. -
Cup dosing: 11.3 mL ibuprofen; cup marked every 2.5 mL.
Prefer syringe for accuracy; if only cup, round to nearest readable mark per policy—11.25 ≈ 11 mL or 12.5 mL is unsafe; use syringe (ISMP). -
High-alert microdose: 0.031 mL required; device min 0.1 mL.
Do not round to 0.0 or 0.1—dilute to a measurable volume per policy, then recalc final concentration.
Professor’s note: If rounding changes **therapeutic intent** (e.g., ER split, big swings on high-alert meds), it’s not rounding—it’s an error. On NCLEX, answers that respect device limits, dosage forms, and policy nearly always win.
FAQs
What’s the general NCLEX rule for rounding IV mL/hr?
Unless specified, round to whole mL/hr for standard pumps. Use decimal precision only if ordered or if a syringe pump requires it, per unit policy (Upstate.edu).
Do I ever round gtt/min to a decimal?
No. You can’t give a fraction of a drop. Round to the nearest whole gtt/min; choose microdrip (60 gtt/mL) for small volumes (Bergen.edu).
How should I round small pediatric liquid doses?
Match the syringe graduation: 0.1 mL in general peds; 0.01 mL in NICU/high-precision settings. Use metric devices only and verify MDD (ISMP, AAP links above).
Key Takeaways
- Round to what the device can deliver: tablets → scored fractions; syringes → 0.1 or 0.01 mL; pumps → whole mL/hr unless ordered otherwise; gravity drips → whole gtt/min.
- Pediatrics often requires micro-rounding and MDD checks; adjust concentration rather than “force” a round.
- Respect dosage forms (no splitting ER/EC) and use metric-only devices to reduce errors (ISMP/AAP/FDA).
- Build speed with targeted practice and NGN case formats that demand precise math.