If we were together in class right now, I’d start with a question: “What’s the first thing you verify before any pediatric dose?” (Answer: an up-to-date weight in kilograms.) From there, pediatric med math becomes a pattern: convert → compare to mg/kg (or mcg/kg/min) → check maximum daily dose (MDD) → translate to a safe volume or rate. I’ll walk you through the same approach I use when teaching NGN prep—steady, unit-driven, and obsessively safety-checked.
Why the fuss? Children have smaller volumes of distribution and many meds with narrow therapeutic ranges. A rounding slip or a missed MDD can push a patient into toxicity. On NCLEX, that means you must set up the math so that units cancel themselves, and you must recognize red-flag answers (e.g., a 25 mL oral volume for a toddler). In your practice, it means fewer near-misses and more confident, timely care.
Here’s the plan: I’ll give you a clear “unit-canceling” method (dimensional analysis), show you where rounding typically lands in real policy, and then we’ll work through 20 common scenarios—oral liquids, tablets, mL/hr, gtt/min, and mcg/kg/min titrations. I’ll also point you to authoritative references as we go—for example, dosing tables from the American Academy of Pediatrics (acetaminophen; ibuprofen) and maintenance-fluid formulas from academic sources (University of Iowa; UTMB). Keep this page open while you practice—and use our related NCLEX pieces to build speed and judgment.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- Pediatric Dosing Fundamentals: Units, Conversions & Safety Checks
- Dimensional Analysis & Common Formulas (with Rounding Rules)
- 20 Practice Scenarios with Answers & Rationale
- FAQs
- Key Takeaways
- Further Reading
Pediatric Dosing Fundamentals: Units, Conversions & Safety Checks
My teaching mantra: “Let the units do the thinking.” Here’s the six-step workflow I drill with students:
- Verify weight in kilograms
- If documentation is in pounds, convert: lb ÷ 2.2 = kg.
- Re-weigh if the value is old or clinically suspect. AAP guidance to parents also emphasizes weight-based dosing and using proper devices—not household teaspoons (AAP: Using Liquid Medicines).
- Translate the order to mg/kg (or mcg/kg/min)
- Ex: “amoxicillin 25 mg/kg/day divided q12h” → compute daily mg from weight → divide by number of doses.
- Check the MDD (maximum daily dose)
- Compare the calculated total to the pediatric MDD from your policy/drug reference. If over, cap at MDD and clarify.
- Pick the right concentration
- Oral: use the bottle label (e.g., 160 mg/5 mL).
- IV: work from the prepared/standardized infusion (e.g., 400 mg in 250 mL).
- Choose the delivery rate
- Pumps: compute mL/hr.
- Gravity: compute gtt/min using the drop factor. Academic resources consistently note standard macrodrip sets (10–20 gtt/mL) vs microdrip sets at 60 gtt/mL (AVC.edu flow-rate guide; Bergen.edu pharmacology math).
- Round safely & document
- Liquids: many units round oral syringes to the nearest 0.1 mL; micro-infusions may round to 0.01 mL per policy.
- Gravity drip calculations often round to whole gtt/min (see university dosage-math guides, e.g., Upstate.edu).
- Follow local policy if the stem doesn’t specify.
Professor’s note: In my courses, I require students to write the **goal unit** at the far right (e.g., “mL to give”) and then stack conversion factors so labels cancel diagonally. If a label doesn’t cancel, you’re missing a step—fix that before any arithmetic.
Pair this core with targeted refreshers: for infusion math, see IV Drip Rates & Infusions (2025). To sharpen NGN clinical judgment, read How to Read NGN Case Stems (2025).
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Dimensional Analysis & Common Formulas (with Rounding Rules)
The unit-canceling method
Write the quantity you want, then multiply by equivalences so units cancel:
[ \text{mL to give}=\frac{\text{ordered mg}}{\text{available mg}}\times\text{available mL} ]
Oral liquid example
Order: 150 mg; bottle: 160 mg/5 mL
[
150\ \text{mg}\times\frac{5\ \text{mL}}{160\ \text{mg}}=4.69\ \text{mL}\rightarrow \mathbf{4.7\ \text{mL}}
]
IV pump rates (mL/hr)
[ \text{mL/hr}=\frac{\text{total mL}}{\text{hours}} ] If the order says “infuse 20 mL over 30 min,” then (20/0.5=\mathbf{40\ mL/hr}).
Gravity drip rates (gtt/min)
[ \text{gtt/min}=\frac{\text{mL/hr}\times\text{drop factor (gtt/mL)}}{60} ] Microdrip sets are typically 60 gtt/mL (AVC.edu).
Weight-based continuous infusions (mcg/kg/min or units/kg/hr)
[ \text{mL/hr}=\frac{\text{dose}\times\text{weight}\times 60}{\text{concentration (per mL)}} ]
Professor’s note (safety): For pediatrics, order entry and labels should use **metric units** (not “teaspoons”), and weight-based logic (mg/kg) should be visible on the order. These are longstanding best practices promoted by medication-safety organizations like ISMP (ISMP Best Practices; ISMP: Oral solution errors).
Maintenance fluids (the 4-2-1 rule)
The traditional approach derives from Holliday–Segar. Many academic resources teach: 4 mL/kg/hr for the first 10 kg, 2 mL/kg/hr for the next 10 kg, 1 mL/kg/hr for each kg thereafter (University of Iowa; UTMB). Children’s Hospital of Philadelphia also outlines maintenance calculations within clinical pathways (CHOP clinical pathway).
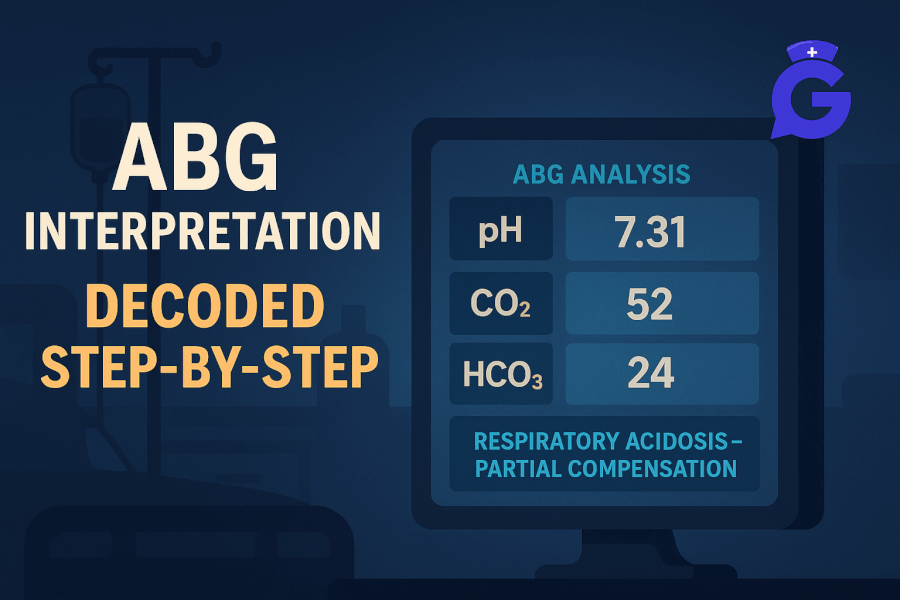
To round out med-safety instincts, skim drug windows and monitoring in Therapeutic Drug Levels (2025), and practice ABGs to recognize perfusion/ventilation trends during titrations: ABG Interpretation (2025).
20 Practice Scenarios with Answers & Rationale
Assume typical rounding unless noted. On NCLEX, follow the stem’s rounding instruction when provided.
-
Amoxicillin oral suspension: 25 mg/kg/day divided q12h; weight 14.2 kg; 400 mg/5 mL
Daily = 25×14.2=355 mg → per dose = 177.5 mg → volume = (177.5/400 × 5 = \mathbf{2.2\ mL}). -
Ibuprofen: 10 mg/kg/dose q6h PRN; weight 22.5 kg; 100 mg/5 mL
Dose = 225 mg → volume = (225/100 × 5 = 11.25) → 11.3 mL. Typical pediatric guidance caps daily ibuprofen at ~40 mg/kg/day; check local policy/AAP tables (AAP ibuprofen table). -
Acetaminophen: 15 mg/kg/dose q6h; weight 18.6 kg; 160 mg/5 mL
Dose = 279 mg → volume (= 279/160 × 5 = 8.72) → 8.7 mL. Confirm MDD per label/policy; AAP provides weight-based tables for safe use (AAP acetaminophen table). -
IV antibiotic infusion volume: 20 mL over 30 min
Rate = (20/0.5 = \mathbf{40\ mL/hr}). -
Maintenance fluids (4-2-1): 18 kg
10 kg×4=40; remaining 8 kg×2=16 → 56 mL/hr (University of Iowa). -
Gentamicin: 2.5 mg/kg/dose q8h; weight 7.8 kg; 10 mg/mL
Dose = 19.5 mg → volume (= 19.5/10 = \mathbf{1.95\ mL}) (use precise syringe). -
Dopamine infusion: 5 mcg/kg/min; 15.5 kg; 400 mg in 250 mL (=1600 mcg/mL)
Rate (= \frac{5×15.5×60}{1600} \approx \mathbf{2.91\ mL/hr}). -
Epinephrine IM (anaphylaxis): 0.01 mg/kg of 1 mg/mL; weight 32 kg; max 0.3 mg
Calculated 0.32 mg → cap at 0.3 mg = 0.3 mL (dose capping per policy). -
Heparin infusion: 18 units/kg/hr; 11.8 kg; 25,000 units/250 mL (=100 units/mL)
Units/hr = 212.4 → rate (= 212.4/100 = \mathbf{2.12\ mL/hr}). -
Insulin infusion (DKA): 0.1 units/kg/hr; 28.4 kg; 1 unit/mL
Rate (= 0.1×28.4 = \mathbf{2.84\ mL/hr}). -
Vancomycin: 15 mg/kg q6h; 19.2 kg; withdraw from 50 mg/mL stock, dilute to 100 mL and infuse over 1 hr
Dose = 288 mg → withdraw (= 288/50 = \mathbf{5.76\ mL}) → infuse 100 mL/hr. -
Prednisone tablets: 1 mg/kg/day; 17.6 kg; 5 mg tablets
Daily ≈ 17.6 mg → use 17.5 mg (3½ × 5 mg) per policy/availability. -
Ampicillin reconstituted: 125 mg; vial concentration 250 mg/mL
Volume (= 125/250 = \mathbf{0.50\ mL}). -
Norepinephrine: 0.05 mcg/kg/min; 20 kg; 4 mg in 250 mL (=16 mcg/mL)
Rate (= \frac{0.05×20×60}{16} = \mathbf{3.75\ mL/hr}). -
Sodium bicarbonate: 1 mEq/kg/dose; 12 kg; 1 mEq/mL
Volume (= 12/1 = \mathbf{12\ mL}). -
Acetaminophen suppositories: 15 mg/kg; 13.4 kg; 80 mg and 120 mg strengths
Dose = 201 mg → use 200 mg (120 mg + 80 mg), within typical ±10% rounding—confirm policy. -
Digoxin elixir: 10 mcg/kg/day divided q12h; 9.3 kg; 50 mcg/mL
Daily = 93 mcg → per dose 46.5 mcg → volume (= 46.5/50 = \mathbf{0.93\ mL}). -
Morphine IV: 0.05 mg/kg/dose; 16.2 kg; 2 mg/mL
Dose = 0.81 mg → volume (= 0.81/2 = \mathbf{0.41\ mL}). -
Phenytoin loading: 15 mg/kg over 2 hr; 25 kg; stock 50 mg/mL; dilute to 50 mL
Total = 375 mg → withdraw (= 375/50 = 7.5) mL into bag → infuse 25 mL/hr. -
Normal saline bolus: 20 mL/kg over 30 min; 13.2 kg
Bolus = 264 mL → rate (= 264/0.5 = \mathbf{528\ mL/hr}).
Professor’s note (exam tip): When the arithmetic is done, ask: “Does the **volume** make sense for this child and route?” If not, re-check weight units, bottle concentration, and whether an **MDD** or rate limit applies. That five-second pause prevents the majority of calculation errors.
FAQs
What’s the safest first step in pediatric med math?
Confirm a current weight in kilograms. Then set up the problem with dimensional analysis so units cancel cleanly.
How should I round pediatric liquid doses on NCLEX?
If the stem doesn’t specify, use typical practice: oral syringes to the nearest 0.1 mL; micro-infusions may need 0.01 mL per policy. Gravity drip answers are commonly whole gtt/min (see Upstate.edu).
Where can I verify OTC fever-reducer doses for children?
Use AAP’s consumer tables for acetaminophen and ibuprofen (AAP acetaminophen; AAP ibuprofen) and your facility’s formulary.
How do I avoid oral liquid measurement errors?
Use metric-marked syringes, not kitchen spoons; teach-back is key. See ISMP’s pediatric liquid-med guidance (ISMP) and AAP advice on using liquid medicines (AAP).
Key Takeaways
- Convert to kg, apply mg/kg (or mcg/kg/min), and verify MDD before you round or draw up.
- Dimensional analysis (unit-canceling) catches most errors before they happen.
- Pumps use mL/hr; gravity sets use gtt/min with the stated drop factor (microdrip commonly 60 gtt/mL).
- Build speed with targeted practice and NGN-style judgment prompts—not just calculators.