The Next Gen NCLEX (NGN) rewards how you think—not just what you know. This guide shows a repeatable approach to reading case stems the way a safe new nurse does: identify the right cues, connect them to a priority, choose the safest effective action, and reassess. You’ll learn the common traps, the signal words that change priority, and a pacing plan that fits the exam clock.
Table of Contents
- What Makes NGN Different
- The Clinical Judgment Model in Plain Language
- A Step-by-Step Method for Any NGN Stem
- Signal Words That Change Priority
- Common Traps & How to Avoid Them
- Time Management & Partial Credit
- Mini Walkthroughs (3 Cases)
- Printable Checklist
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge—new quizzes added weekly!
What Makes NGN Different
- Case-based stems present changing information: notes, vitals, labs, orders, and nursing notes.
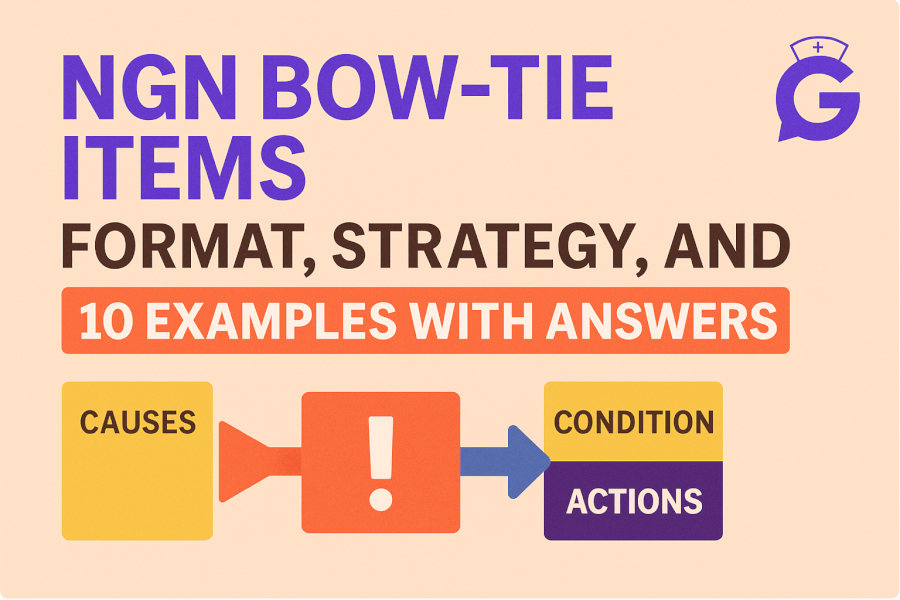
- Multiple scored interactions per case (bow-tie, matrix/grid, trend, highlight).
- Partial credit: selecting relevant cues/actions still earns points even if not perfect.
- Emphasis on clinical judgment over rote recall.
Goal: demonstrate safe, timely decision-making with incomplete data.
The Clinical Judgment Model in Plain Language
The NGN blueprint operationalizes clinical judgment into six steps. Here’s the simple version to apply on every stem:
- Recognize cues — pull the few pieces of data that matter right now.
- Analyze cues — group them into a likely problem pattern.
- Prioritize hypotheses — decide the most urgent issue.
- Generate solutions — list safe, effective nursing actions.
- Take action — do the highest-priority step first.
- Evaluate outcomes — check if the client improved.
If you can state your thinking in one line—“These cues point to hypoxia; first action is oxygen and positioning, then reassess in 10 minutes”—you’re using the model.
A Step-by-Step Method for Any NGN Stem
Use this six-step reading plan like a checklist:
A) Time anchor
Is this initial presentation, post-op Day 1, “worsening over 4 hours,” or “10 minutes after morphine”? Time stamps change urgency and drug effects.
B) Vital signs scan
Read vitals as a trend, not isolated numbers. “RR 26 ↑, SpO₂ 88% ↓, BP low-normal, drowsy” suggests hypoventilation risk; “temp 39.2, HR 118, BP 94/56, confused” suggests sepsis/hypoperfusion.
C) Red-flag cues
Airway/breathing, perfusion, new neuro deficits, anaphylaxis/sepsis patterns, high-alert meds (insulin, opioids, anticoagulants).
D) One-line priority
Write 7–12 words: “Likely hypoxia from opioid sedation; oxygenation is priority.”
E) Safest effective action(s)
Prefer least-invasive, most effective steps you can implement now (positioning, oxygen per protocol, hold medication, frequent reassessment) before calling the provider.
F) Reassessment plan
Specify what you’ll check and when: SpO₂, RR, breath sounds, mentation, urine output, MAP—usually within 10–30 minutes.
This method maps directly to bow-tie (problem → actions → parameters) and matrix items (select-all cues/actions/rationales).
Signal Words That Change Priority
These words in stems should make you pause:
- Increasing/worsening/escalating: trend toward instability; act now.
- New/acute/sudden: often outranks chronic issues.
- Post-op/first 24 hours: watch airway/bleeding/pain control complications.
- After medication: link adverse effects (e.g., morphine → hypoventilation).
- Confused/drowsy/unresponsive: neuro changes; check oxygenation/glucose and safety.
- Oliguria or MAP < 65: perfusion problem; fluids/pressors per orders.
- High-risk diagnosis: DKA, sepsis, PE, preeclampsia—prioritize stabilization.
Common Traps & How to Avoid Them
- Pretty numbers: “Normal-ish” values may still be wrong for this client (SpO₂ 92% in pneumonia with rising RR can be unsafe).
- Do-everything lists: The best answers are targeted, not long checklists.
- Provider-first reflex: Do the immediate nursing action you can implement safely before making the call.
- Cue hoarding: Selecting too many unrelated cues loses points; pick the most relevant few.
- Routine over priority: Don’t grab vitals before opening the airway in clear respiratory compromise.
For category expectations and weights, review NCLEX categories and an instability primer:
- https://goodnurse.com/article/2/nclex-categories
- https://goodnurse.com/article/112/physiological-adaptation-definitions-key-concepts-and-mnemonics
Time Management & Partial Credit
- Macro pacing: ~2 minutes per scored interaction; don’t stall on one grid.
- Micro cycle: Read stem (20–30 s) → mark cues (20–30 s) → choose action(s) (30–40 s) → quick sanity check (10 s).
- Partial credit mindset: If stuck, select the clearly relevant cues/actions; avoid random extras.
- Flag and move: If a later screen depends on earlier data, commit to your best rationale and keep the pace.
Mini Walkthroughs (3 Cases)
Case 1 — Post-op hypoxia
- Stem: 64-year-old post-op client, RR 26, SpO₂ 88% on room air, shallow breaths; drowsy 30 minutes after morphine.
- Cues to select: SpO₂ 88%, shallow respirations, recent opioid, drowsiness.
- Priority hypothesis: Hypoventilation with hypoxia.
- Actions: Elevate HOB; apply oxygen per protocol; encourage deep breathing/incentive spirometry; prepare to reduce opioid dose or consider naloxone per orders if indicated; continuous pulse oximetry.
- Evaluate: Reassess SpO₂, RR, sedation score in 10–15 minutes; document response.
Case 2 — Suspected sepsis
- Stem: 79-year-old with UTI; temp 39.1 °C, HR 118, BP 94/56, RR 24, new confusion; lactate pending.
- Cues to select: Fever, tachycardia, hypotension, altered mentation, suspected infection.
- Priority hypothesis: Sepsis with possible hypoperfusion.
- Actions: Obtain cultures if not yet drawn; start broad-spectrum antibiotics per order; begin IV fluids; monitor urine output; apply oxygen if hypoxic; trend MAP/mentation.
- Evaluate: Repeat vitals, mentation, urine output every 15–30 min initially; follow lactate; escalate per protocol.
Case 3 — Hyperkalemia on telemetry
- Stem: Client with CKD: K⁺ 6.1 mEq/L, peaked T-waves, HR 54, mild weakness; new orders include insulin with dextrose and sodium polystyrene; telemetry alarm pending.
- Cues to select: K⁺ 6.1, peaked T-waves, bradycardia, CKD.
- Priority hypothesis: Risk for dysrhythmia due to hyperkalemia.
- Actions: Place on continuous cardiac monitoring; anticipate giving insulin with dextrose per order; verify IV access; prepare calcium gluconate per protocol if instability; hold potassium supplements.
- Evaluate: Repeat potassium and EKG; watch for rhythm changes and hypoglycemia.
For integrating NGN practice into a study plan, see weekly pacing ideas:
Printable Checklist
- Identify timeline and trend words.
- Mark the red-flag cues (airway, perfusion, neuro, sepsis, high-alert meds).
- Write one-line priority.
- Choose 1–2 safest effective actions you can do now.
- Note what to reassess and when.
- If stuck, pick the clearly relevant options and move on.
FAQs
How many cues should I select on a matrix item?
Only the cues that drive your priority for this case. Adding unrelated cues lowers your score.
What if two actions seem right?
Choose the action that best addresses the highest-priority problem and is safe to implement immediately.
How much time should I spend per screen?
About 2 minutes. If you hit ~3 minutes, make your best clinical choice and proceed.
Do I need to memorize labs?
Yes—focus on ABGs, CBC, BMP, hepatic/renal panels, and therapeutic drug levels for high-alert meds.
Will partial credit save me if I miss a key action?
It helps, but you still need the priority action. Practice recognizing red-flag patterns to avoid that miss.