Hypernatremia Nursing Care Plan
Hypernatremia shows up fast—dry mucosa, intense thirst, agitation or lethargy—and students often worry most about which fluid to hang and how quickly to lower sodium. In precepting med-surg and step-down, I’ve seen the best outcomes when nurses use a simple framework: confirm hypotonic hypernatremia, estimate the free-water deficit, choose fluids that match the physiology (DI vs dehydration vs osmotic diuresis), and correct slowly to avoid cerebral edema. This NGN-ready guide gives you a practical blueprint with prioritized nursing diagnoses, SMART outcomes, and interventions with rationales you can chart today.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Pathophysiology of Hypernatremia
Hypernatremia (commonly Na⁺ > 145 mEq/L; verify your lab range) usually reflects a loss of free water in excess of sodium. When plasma osmolality rises, water leaves brain cells, causing cellular dehydration—manifesting as thirst, irritability or lethargy, confusion, myoclonus, and seizures in severe cases. Typical drivers include:
- Water loss > Na⁺ loss: fever, sweating, diarrhea, osmotic diuresis (e.g., hyperglycemia), loop diuretics without adequate free water.
- Diabetes insipidus (DI): central or nephrogenic—impaired ADH signaling causes large volumes of dilute urine and rapid free-water loss.
- Na⁺ gain (less common): hypertonic sodium bicarbonate, seawater ingestion, or iatrogenic hypertonic saline.
Initial priorities: 1) protect the brain (frequent neuro checks, seizure precautions), 2) restore intravascular volume first if hypovolemic (isotonic saline), 3) then replace free water gradually (D5W or 0.45% NS per order), and 4) treat the cause (e.g., desmopressin for central DI, hold offending meds, address hyperglycemia). For patient-friendly overviews, see MedlinePlus (NIH/NLM); for clinical background, refer to NCBI Bookshelf.
Quick Clinical Framework (bedside)
- Confirm hypotonic hypernatremia: check serum osmolality and rule out hyperglycemia-related shifts.
- Assess volume status: tachycardia, hypotension, dry mucosa (hypovolemia) vs. euvolemia in DI.
- Urine studies: high urine output with low urine osmolality suggests DI; osmotic diuresis shows high urine glucose/osm.
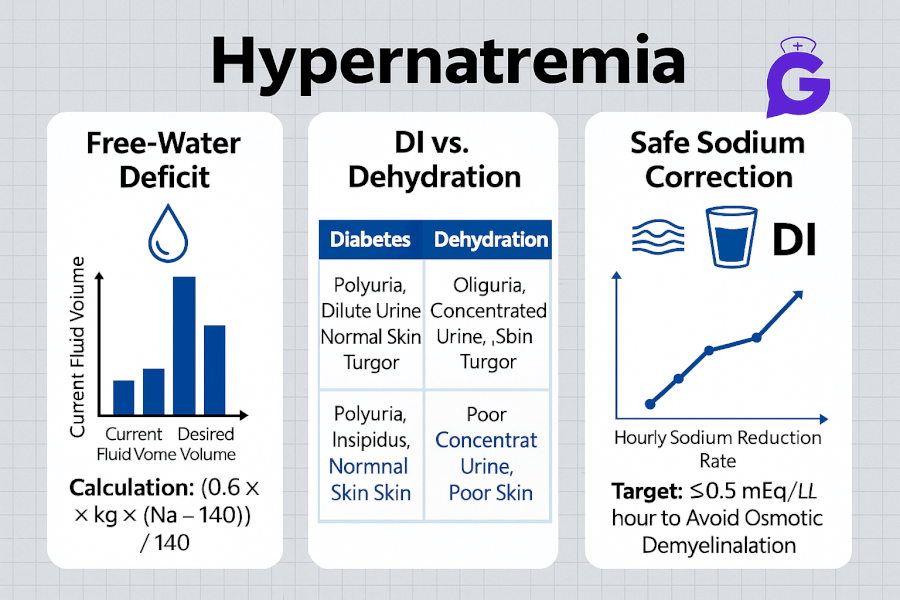
- Estimate free-water deficit:
Deficit ≈ TBW × [(Na⁺/140) − 1](TBW ~ 0.6 × weight (kg) men; ~0.5 women; adjust for age/comorbidity). - Correct slowly: common target is ≤ ~10–12 mEq/L fall in 24 h (follow provider and facility protocol).
Reinforce your clinical judgment with NGN resources: NGN Med-Surg Case Studies, electrolyte patterns in Electrolytes Cheat Sheet, and quick refreshers in Electrolyte Imbalances Made Easy.
Nursing Care Plans for Hypernatremia
Prioritize neurologic safety and safe correction while addressing the underlying cause. Individualize values and orders per provider and protocol.
Nursing Diagnosis: Risk for Injury (seizures/falls) related to neuronal dehydration
| Category | Details |
|---|---|
| Related to | Cerebral cellular dehydration from hyperosmolality; acute mental status changes |
| As evidenced by | Agitation or lethargy, confusion, myoclonus, seizures, positive fall-risk screen |
| Desired Outcomes | Remains free of injury; no seizures; neuro status improves toward baseline as Na⁺ declines at a safe rate. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Institute seizure precautions; perform frequent neuro checks; supervise ambulation. | Reduces injury risk during neurologic instability. |
| Escalate for active seizures or declining airway; ensure rescue meds and equipment are available. | Supports rapid stabilization if neurologic deterioration occurs. |
| Avoid overly rapid Na⁺ correction; trend serum Na⁺ and osmolality per protocol (e.g., q4–6h initially). | Prevents cerebral edema from rapid osmotic shifts. |
Nursing Diagnosis: Deficient Fluid Volume (dehydration) or Risk for Imbalanced Fluid Volume
| Category | Details |
|---|---|
| Related to | Inadequate free-water intake, excessive insensible/GI/renal losses, DI (central or nephrogenic) |
| As evidenced by | Dry mucosa, orthostasis, tachycardia, poor skin turgor, high serum osmolality; in DI—polyuria with low urine osmolality |
| Desired Outcomes | Stable hemodynamics; urine output ≥0.5–1 mL/kg/hr; Na⁺ trends down safely; symptoms improve within 24–48 h. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| If hypovolemic, start isotonic saline per order to restore perfusion, then transition to hypotonic fluids (e.g., D5W or 0.45% NS) to replace free water. | Volume first prevents hemodynamic collapse; hypotonic solutions correct the water deficit afterward. |
| Measure strict I&O and daily weights; monitor urine osmolality and specific gravity if available. | Tracks fluid status and response to therapy, especially in DI/osmotic diuresis. |
| Address the cause: administer desmopressin (DDAVP) for central DI per order; manage hyperglycemia; review/hold contributing meds. | Treating the driver prevents recurrent free-water loss and rebound hypernatremia. |
Nursing Diagnosis: Deficient Knowledge (hypernatremia safety & prevention)
| Category | Details |
|---|---|
| Related to | Unfamiliarity with fluid plans, DI management, and signs of neurologic compromise |
| As evidenced by | Questions about thirst control, fluid choices, desmopressin use, and when to seek care |
| Desired Outcomes | Patient/family teach back fluid/replacement plan, medication timing, and return precautions before discharge. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Explain safe correction: typical goal ≤ ~10–12 mEq/L fall in 24 h (provider/facility protocol may be stricter). | Sets expectations and reduces risk of overly rapid correction. |
| Review DI plans if applicable: desmopressin administration, missed-dose actions, and daily weight/fluid logs. | Improves adherence and early detection of worsening polyuria or recurrence. |
| Teach return precautions: worsening confusion, severe headache, vomiting, seizures, or reduced urine output. | Prompts timely escalation for neurologic decline or renal compromise. |
NGN Clinical Judgment Pearls
- Order of operations: If hypovolemic, restore circulation with isotonic saline before free-water replacement.
- Pick the right hypotonic: D5W behaves like free water; 0.45% NS is hypotonic but provides some sodium—follow orders and monitor closely.
- Watch the rate: Too-rapid decline in Na⁺ can cause cerebral edema; schedule Na⁺ checks and adjust infusion rates per protocol.
- DI clue: High urine output with low urine osmolality; rapid response to desmopressin supports central DI.
Frequently Asked Questions (FAQ)
How do you calculate the free-water deficit?
A common estimate is TBW × [(Serum Na⁺ / 140) − 1], where TBW ≈ 0.6 × weight (kg) for men and ≈ 0.5 for women (adjust for age/comorbidities). Replace gradually while trending Na⁺.
Which IV fluids are used for hypernatremia?
If hypovolemic, start with 0.9% NS to restore perfusion; then replace free water with D5W or 0.45% NS per provider order. In DI, pair fluids with the appropriate therapy (e.g., desmopressin for central DI).
How quickly should sodium be corrected?
Follow provider/facility protocol. Many targets limit the fall in Na⁺ to ≈10–12 mEq/L in 24 hours (or stricter for chronic hypernatremia) to minimize cerebral edema risk.
What labs should I trend?
Serum Na⁺ and osmolality, glucose (if osmotic diuresis), BUN/Cr, and—if DI suspected—urine osmolality/specific gravity and volumes. Document I&O and daily weights.
Further Reading
- Hyperkalemia Nursing Care Plan (First-Hour Priorities)
- Hypokalemia Nursing Care Plan (Safe IV K⁺ & Mg²⁺ Co-Repletion)
- Hypercalcemia Nursing Care Plan
- Hypocalcemia Nursing Care Plan
- Primary Hyperparathyroidism Nursing Care Plan
- Hypercalcemia of Malignancy Nursing Care Plan
- Calcium Kidney Stones (Nephrolithiasis) Nursing Care Plan
- ABG Interpretation: 15 Practice Cases
- NGN Med-Surg Case Studies
- Electrolyte Imbalances Made Easy
- Electrolytes Cheat Sheet (Na⁺/K⁺/Ca²⁺/Mg²⁺ Patterns)