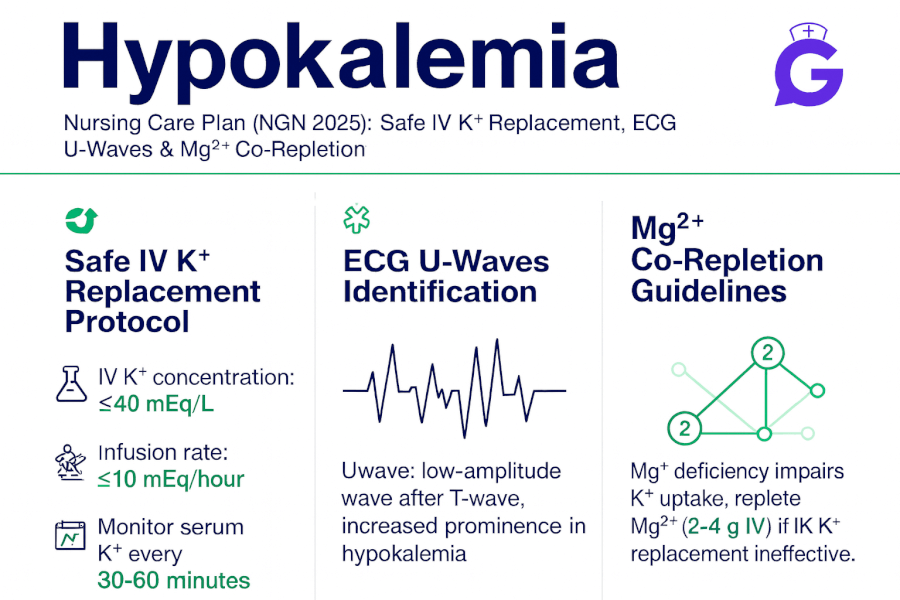
Seeing flattened T waves, muscle cramps, and a potassium of 2.9? I’ve watched students panic here—and they don’t need to. In this NGN-ready guide, I’ll walk you through hypokalemia in a calm, structured way: quick pathophysiology, prioritized nursing diagnoses with SMART outcomes, and interventions with rationales you can chart immediately. We’ll cover safe IV/PO potassium replacement, why magnesium matters, and how to protect against dysrhythmias—plus simple teaching points patients actually remember.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances (2025) - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Pathophysiology of Hypokalemia
Hypokalemia (often < 3.5 mEq/L; confirm your lab’s range) decreases extracellular K⁺, hyperpolarizing cell membranes and slowing repolarization. Typical causes include GI losses (vomiting, diarrhea, laxative misuse), renal losses (loop/thiazide diuretics, hyperaldosteronism), intracellular shifts (alkalosis, insulin/β-agonists), inadequate intake, and magnesium deficiency (impairs Na⁺/K⁺-ATPase and ROMK, making K⁺ repletion refractory). ECG findings can show flattened T waves, ST depression, and U waves, with risk of atrial/ventricular dysrhythmias—especially in digoxin users. For concise clinical overviews, see NCBI Bookshelf (NIH) and Cleveland Clinic.
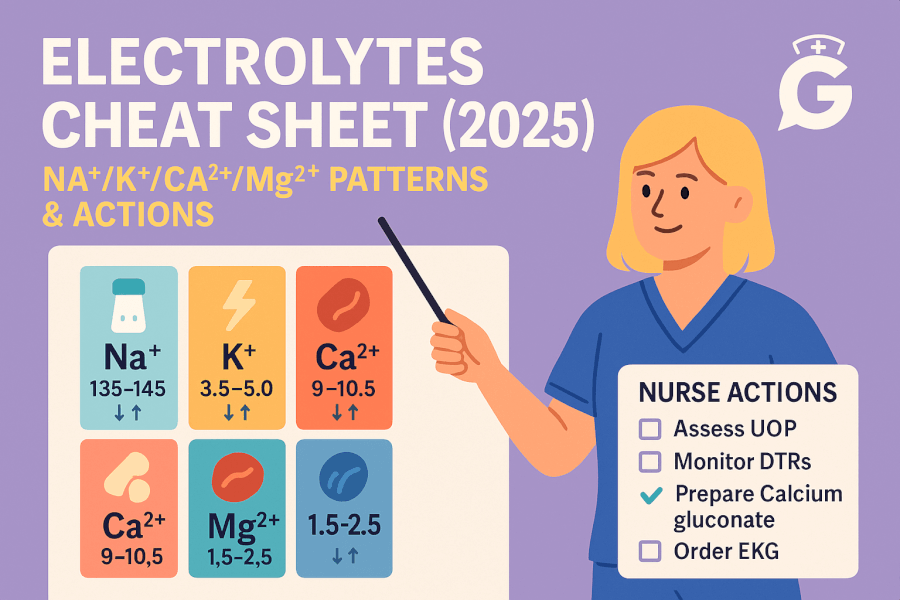
Pair this with our electrolyte & calcium cluster for fast differentials and teaching aids: Electrolyte Imbalances Made Easy, Electrolytes Cheat Sheet, Hypercalcemia Care Plan, Hypocalcemia Care Plan, Primary Hyperparathyroidism, Hypercalcemia of Malignancy, Calcium Kidney Stones.
Nursing Care Plans for Hypokalemia
Use these prioritized nursing diagnoses, outcomes, and interventions with rationales to individualize care for your patient and setting.
Nursing Diagnosis: Risk for Decreased Cardiac Output (dysrhythmias)
| Category | Details |
|---|---|
| Related to | Prolonged repolarization and conduction delay from low extracellular potassium |
| As evidenced by | Flattened T waves, ST depression, U waves; ectopy or bradyarrhythmias; K⁺ below target |
| Desired Outcomes | Maintains stable rhythm; ECG changes improve as K⁺ rises; K⁺ reaches provider-set target within 6–24 hrs without adverse effects. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Initiate continuous cardiac monitoring; obtain baseline and follow-up 12-lead ECGs. | Detects dysrhythmias and documents resolution with repletion. |
| Administer PO or IV potassium per protocol using an infusion pump; verify renal function and urine output. | Safe replacement reduces arrhythmia risk while preventing iatrogenic hyperkalemia/AKI. |
| Replete magnesium if low; check K⁺ and Mg²⁺ every 2–4 hrs initially based on severity. | Hypomagnesemia makes hypokalemia refractory; co-replacement speeds correction. |
Nursing Diagnosis: Risk for Injury (weakness, cramps, falls)
| Category | Details |
|---|---|
| Related to | Skeletal muscle weakness from low K⁺; orthostatic changes; cramps |
| As evidenced by | Generalized weakness, reduced hand-grip, gait instability, fatigue |
| Desired Outcomes | Free from falls/injury; reports improved strength within 24–48 hrs as K⁺ normalizes. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Implement fall precautions; assist with ambulation until strength returns. | Prevents injury during transient neuromuscular weakness. |
| Assess meds contributing to losses (loop/thiazide diuretics, laxatives) and collaborate on adjustments. | Addresses ongoing losses to maintain correction. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Deficient Knowledge (replacement safety & prevention)
| Category | Details |
|---|---|
| Related to | Unfamiliarity with K⁺ dosing, magnesium co-repletion, diet, and medication interactions |
| As evidenced by | Questions about IV rates, tablet instructions, salt substitutes, and follow-up labs |
| Desired Outcomes | Patient/family teach back home plan: correct dosing, when to call, and triggers for repeat labs/ECG. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach safe IV/PO use: infusion pump only; typical rates (e.g., ≤10 mEq/hr peripheral; ≤20 mEq/hr central with monitoring) per facility policy; do not crush ER tablets; take PO K⁺ with food/water. | Prevents phlebitis, arrhythmias, and GI irritation; reinforces local safety standards. |
| Explain magnesium’s role and plan for co-repletion if ordered. | Improves success of K⁺ correction and reduces recurrence. |
| Review diet per provider (renal vs. non-renal): potassium-rich foods if appropriate; avoid unnecessary laxatives; discuss salt substitutes and drug interactions (e.g., ACEi/ARB, K-sparing diuretics). | Balances intake with comorbidities and medication regimen. |
Frequently Asked Questions (FAQ)
Why won’t potassium correct if magnesium is low?
Magnesium deficiency increases renal K⁺ wasting and impairs cellular uptake, making hypokalemia refractory. Replacing Mg²⁺ first (or concurrently) is often required for K⁺ to stabilize.
What ECG changes suggest hypokalemia?
Flattened or inverted T waves, ST depression, and prominent U waves; severe cases can trigger atrial/ventricular ectopy and tachyarrhythmias.
What are typical safe IV potassium infusion rates?
Follow your facility’s protocol. Common practice: ≤10 mEq/hr via peripheral line; up to 20 mEq/hr via central line with continuous monitoring. Always use a pump and recheck labs.
Any PO tips for patients?
Take with food and a full glass of water; do not crush extended-release tablets; report palpitations, worsening weakness, or muscle cramps.
Further Reading
- Electrolyte Imbalances Made Easy: Mnemonics (2025)
- Electrolytes Cheat Sheet (2025): Na⁺/K⁺/Ca²⁺/Mg²⁺ Patterns
- ABG Interpretation: 15 Practice Cases (with Rationale)
- NGN Med-Surg Case Studies: Physiological Adaptation
- Hypercalcemia Nursing Care Plan (2025)
- Hypocalcemia Nursing Care Plan (2025)
- Primary Hyperparathyroidism Nursing Care Plan (2025)
- Hypercalcemia of Malignancy Nursing Care Plan (2025)
- Calcium Kidney Stones (Nephrolithiasis) Nursing Care Plan (2025)
If you want the complete, up-to-date breakdown of AI for NCLEX prep + nursing school—with independent university study metrics—use this master guide: The Ultimate Guide to AI for NCLEX Preparation and Nursing School.