In clinical, hypocalcemia can look scary—tingling around the mouth, muscle cramps, positive Trousseau/Chvostek signs, even laryngospasm or seizures. If you’ve ever stared at a blank care plan wondering where to start, you’re not alone. In this NGN-ready guide I’ll walk you through the essentials: quick pathophysiology, prioritized nursing diagnoses with SMART outcomes, and step-by-step interventions with rationales. You’ll learn what to do first (and why), how to prevent complications, and how to confidently teach patients and families. Keep this handy for pre-conference, simulation, and NCLEX prep.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- Pathophysiology of Hypocalcemia
- Nursing Care Plans (Diagnoses, Outcomes, Interventions & Rationales)
- FAQs
- Further Reading
- References
Pathophysiology of Hypocalcemia
Hypocalcemia is generally defined as serum calcium below the normal range (often < 8.5 mg/dL; confirm with your lab’s reference). Common etiologies include hypoparathyroidism (post-thyroidectomy, autoimmune), vitamin D deficiency, chronic kidney disease, acute pancreatitis, magnesium deficiency, and massive transfusion (citrate binding). Low ionized calcium increases neuromuscular excitability, leading to tetany, laryngospasm, seizures, and prolonged QT on ECG. Severe or symptomatic cases are medical emergencies that may require IV calcium (typically calcium gluconate) while the underlying cause is corrected (Cleveland Clinic).
Pair this with its clinical counterpart to master differentials: see our Hypercalcemia Nursing Care Plan (2025).
Strengthen clinical reasoning with ABG Interpretation: 15 Practice Cases and apply NGN thinking using NGN Med-Surg Physiological Adaptation Case Studies.
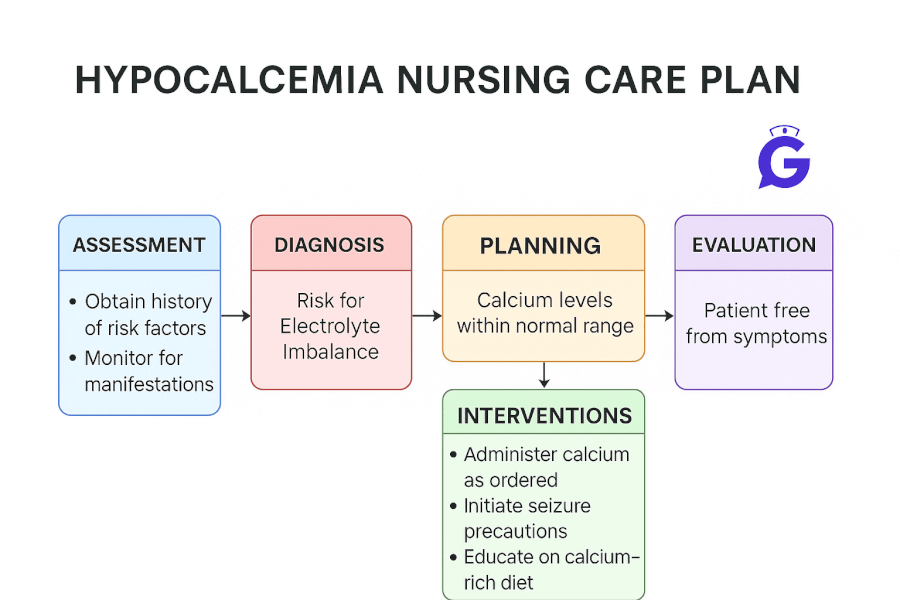
Nursing Care Plans for Hypocalcemia
Below are high-yield nursing diagnoses with SMART outcomes, interventions, and rationales you can adapt to your patient.
Nursing Diagnosis: Risk for Ineffective Airway Clearance (laryngospasm)
| Category | Details |
|---|---|
| Related to | Neuromuscular irritability from low ionized calcium (post-op neck surgery, acute hypocalcemia) |
| As evidenced by | (Risk factors) Positive Trousseau/Chvostek signs, hoarseness/stridor, tingling peri-oral, recent thyroid or parathyroid surgery |
| Desired Outcomes | Maintains patent airway; SpO₂ ≥ 94%; no stridor; ionized calcium normalized per provider targets within 12–24 hrs. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Place airway equipment and calcium gluconate at bedside per protocol; monitor for stridor/hoarseness post-thyroidectomy. | Laryngospasm can rapidly obstruct the airway; early access to therapy reduces morbidity. |
| Continuous pulse oximetry; elevate HOB; provide humidified O₂ if ordered. | Optimizes oxygenation during episodes of airway irritability. |
| Verify labs (ionized Ca²⁺, Mg²⁺) and collaborate to replace magnesium if low. | Hypomagnesemia impairs PTH release/action and makes hypocalcemia refractory. |
Nursing Diagnosis: Risk for Injury (seizure)
| Category | Details |
|---|---|
| Related to | Tetany and neuromuscular irritability from low calcium; prolonged QT predisposing to dysrhythmia/syncope |
| As evidenced by | (Risk factors) Paresthesias, carpopedal spasm, facial twitching, history of seizures or severe electrolyte disorders |
| Desired Outcomes | Remains free from injury; no seizure activity during hospitalization; ECG shows resolution of QT prolongation as Ca²⁺ normalizes. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Implement seizure precautions (padded rails, suction at bedside, supervised ambulation). | Reduces injury risk during unexpected events. |
| Continuous or frequent ECG monitoring in moderate–severe cases. | Hypocalcemia prolongs QT; monitoring guides escalation if dysrhythmias occur. |
| Administer IV calcium as prescribed for symptomatic or severe hypocalcemia; transition to oral calcium/vitamin D as appropriate. | Rapid correction addresses neuromuscular irritability; maintenance prevents recurrence. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Acute Pain (muscle cramps/paresthesias)
| Category | Details |
|---|---|
| Related to | Neuromuscular excitability and tetany due to low ionized calcium |
| As evidenced by | Muscle cramps, carpopedal spasm, facial twitching, peri-oral tingling, restlessness |
| Desired Outcomes | Reports pain ≤ 3/10 within 24 hrs; reduction in cramps/tetany as Ca²⁺ normalizes; sleeps > 6 hrs/night. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Administer prescribed calcium and vitamin D; evaluate response using symptom diary and labs. | Normalization of calcium reduces neuromuscular irritability and pain. |
| Provide warm packs, guided stretching, and relaxation/breathing techniques. | Non-pharmacologic measures reduce muscle spasm discomfort and anxiety. |
Nursing Diagnosis: Deficient Knowledge
| Category | Details |
|---|---|
| Related to | Unfamiliarity with condition, medication regimen (calcium, vitamin D/calcitriol, magnesium), and when to seek care |
| As evidenced by | Questions about diet, supplements, incision/neck symptoms post-op, adherence concerns |
| Desired Outcomes | Patient/family teach back the home plan (meds, labs, diet, red flags) before discharge; demonstrates correct med timing with meals. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach medication purpose/timing (e.g., calcium carbonate with meals; calcitriol as prescribed) and interactions (avoid taking with high-oxalate foods at the same time). | Correct timing improves absorption and symptom control. |
| Review red flags requiring urgent evaluation: worsening hoarseness/stridor, severe cramps, seizures, syncope, or new palpitations. | Early escalation prevents airway compromise and cardiac complications. |
| Reinforce follow-up labs (ionized Ca²⁺, Mg²⁺, PTH, 25-OH vitamin D) and adherence. | Ongoing evaluation ensures the underlying cause is addressed and therapy titrated. |
Frequently Asked Questions (FAQ)
What is the priority nursing intervention for symptomatic hypocalcemia?
Stabilize and protect the airway, then administer IV calcium (often calcium gluconate) as prescribed. Place airway equipment and calcium at bedside, monitor SpO₂/ECG, and correct contributory magnesium deficiency.
Why does hypocalcemia cause a prolonged QT interval?
Low calcium delays phase-2 myocardial repolarization, producing a prolonged QT on ECG—which can predispose to dysrhythmias. Continuous monitoring is indicated for moderate–severe cases.
What labs should I order when calcium is low?
Obtain ionized calcium, magnesium, PTH, 25-OH vitamin D, and consider renal function. Correct low Mg²⁺ first if present, as it can make hypocalcemia refractory.
Why use calcium gluconate vs. calcium chloride?
Calcium gluconate is less irritating to veins and safer for peripheral administration; calcium chloride contains more elemental calcium but is usually reserved for central lines or codes per protocol.
Why do patients become hypocalcemic after thyroid or parathyroid surgery?
Post-operative hypoparathyroidism (temporary or permanent) reduces PTH secretion, lowering serum calcium. Close monitoring for hoarseness/stridor and peri-oral tingling is essential.
Further Reading
- Hypercalcemia Nursing Care Plan (2025)
- ABG Interpretation: 15 Practice Cases (with Rationale)
- NGN Med-Surg Case Studies: Physiological Adaptation
- NGN Pharmacology Case Studies: 10 Examples with Answers
- NGN Matrix/Grid Items: Format & Strategy