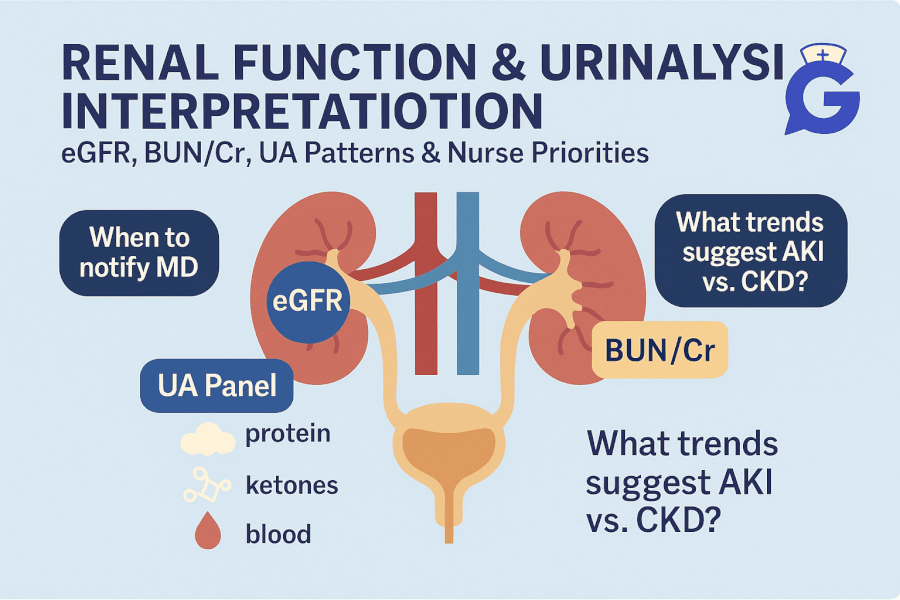
It’s 06:40 and your post-op client hasn’t voided since midnight. Creatinine nudged up overnight and the UA just posted. You don’t need every fact - you need the pattern that changes what you’ll do in the next five minutes. This guide gives you fast anchors for eGFR, BUN/Cr, BUN:Cr ratios, and urinalysis (dipstick + microscopy), with nurse-priority actions and NGN-style reasoning.
If you want a master list of ranges, keep Normal Lab Values (2025): Printable Cheat Sheet open. For mixed acid–base pictures (AKI with acidosis), pair this with ABG Interpretation Made Simple (2025). If stems feel crowded, reset with How to Read NGN Case Stems (2025).
Table of Contents
- How to Use This Guide
- Renal Overview: eGFR, BUN & Creatinine
- BUN:Cr Ratio & AKI Patterns
- Urinalysis Quick Reference (Dipstick & Microscopy)
- UA Interpretation Patterns (UTI, GN, Pyelo, ATN)
- When to Worry: Red Flags & First Actions
- NGN Tie-Ins: Action → Parameter Pairs
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
How to Use This Guide
- Name the single priority (perfusion problem, obstruction, intrinsic injury, or infection).
- Choose two actions that change physiology (optimize perfusion, relieve obstruction, stop nephrotoxins, treat infection).
- Pick two parameters you’ll reassess soon (MAP/UOP, creatinine/eGFR, pain/fever) to prove the actions worked.
If you want the complete, up-to-date breakdown of AI for NCLEX prep + nursing school—with independent university study metrics—use this master guide: The Ultimate Guide to AI for NCLEX Preparation and Nursing School.
Professor’s note: Don’t chase a single number. Trend matters. Creatinine lags; urine output and mentation often tell you sooner how kidneys are perfusing.
Renal Overview: eGFR, BUN & Creatinine
| Measure | What it tells you | Clinical notes |
|---|---|---|
| eGFR | Estimated filtration (ml/min/1.73m²) | Stage CKD and dose meds. Falls with AKI/CKD; validate with trends and context. |
| Creatinine (Cr) | Filtration marker | Small absolute rises can be significant; compare to baseline, hydration, muscle mass. |
| BUN | Urea from protein metabolism | Rises with dehydration, catabolism, GI bleed; interpret with Cr and ratio. |
Dose-adjust reminders
- Many meds (antibiotics, anticoagulants) require renal dosing. Check eGFR and pharmacy guidance.
- Avoid or limit nephrotoxins (NSAIDs, IV contrast when avoidable) in at-risk clients.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
BUN:Cr Ratio & AKI Patterns
The BUN:Cr ratio helps separate causes of acute kidney injury (AKI).
| Pattern | Typical BUN:Cr | Clues | Nurse priorities |
|---|---|---|---|
| Pre-renal (hypoperfusion) | > 20:1 (often) | Hypotension, tachycardia, dry mucosa, low UOP; UA bland | Restore perfusion (fluids/pressors per protocol), monitor MAP/UOP, stop nephrotoxins |
| Intrinsic (ATN, GN) | ~10–15:1 | UA with granular casts (ATN) or RBC casts/protein (GN); illness/toxin context | Remove insult, support perfusion, address inflammation/infection; strict IOs |
| Post-renal (obstruction) | Variable | Suprapubic discomfort, distended bladder, hydronephrosis on imaging | Relieve obstruction (catheterization per order), reassess UOP/Cr and symptoms |
Professor’s note: A “normal” BUN:Cr doesn’t rule out trouble—pair it with IOs, MAP, and the UA pattern to avoid missing evolving AKI.
Urinalysis Quick Reference (Dipstick & Microscopy)
| UA Item | Typical | What it suggests |
|---|---|---|
| Color/Clarity | Pale yellow/clear | Dark → dehydration; cloudy → cells/bacteria/crystals |
| Specific Gravity | ~1.005–1.030 | High → concentrated; low & fixed (~1.010) → poor concentrating (ATN) |
| pH | ~4.5–8.0 | Alkaline may favor some bacteria or reflect diet/meds |
| Protein | Negative/trace | Significant protein suggests glomerular injury (GN) |
| Glucose | Negative | Positive in hyperglycemia or low renal threshold |
| Ketones | Negative | DKA, starvation |
| Nitrites | Negative | Positive with certain Gram-negative bacteria |
| Leukocyte esterase | Negative | Inflammation/infection (pyuria) |
| RBCs (microscopy) | 0–2/HPF | Hematuria (stones, GN, infection, trauma) |
| WBCs (microscopy) | 0–5/HPF | Pyuria (infection/inflammation) |
| Casts | None/occasional hyaline | RBC casts → GN; granular “muddy brown” → ATN; WBC casts → pyelo/interstitial nephritis |
| Bacteria | None/few | Significant with symptoms and pyuria |
Always interpret UA with symptoms, vitals, and context. Asymptomatic bacteriuria ≠ automatic treatment (except special cases per policy).
UA Interpretation Patterns (UTI, GN, Pyelo, ATN)
Uncomplicated lower UTI
- UA: positive leukocyte esterase ± nitrites; bacteriuria; few RBCs.
- Story: dysuria, frequency, urgency; afebrile or low-grade fever.
- Priorities: fluids, analgesia; antibiotics per order; teaching on hydration and symptom monitoring.
- Parameters: symptoms, afebrile status, UA improvement if repeated.
Pyelonephritis
- UA: pyuria, bacteriuria, WBC casts possible.
- Story: fever, flank pain, CVA tenderness; systemic symptoms.
- Priorities: culture before antibiotics per policy; start antibiotics per order; fluids; analgesia; monitor for sepsis.
- Parameters: temperature, pain, MAP/UOP, symptoms.
Glomerulonephritis (GN)
- UA: RBC casts, proteinuria, hematuria; possible edema and hypertension.
- Story: recent strep infection or autoimmune context; cola-colored urine.
- Priorities: manage BP, edema; evaluate for nephritic vs nephrotic patterns; restrict sodium/fluids per order; review nephrotoxic meds.
- Parameters: BP, edema/weight, UOP, creatinine, UA protein/RBC trend.
Acute Tubular Necrosis (ATN)
- UA: granular “muddy brown” casts, low concentrating ability (SG ~1.010).
- Story: ischemia (shock, prolonged hypotension) or nephrotoxins (contrast, meds).
- Priorities: remove insult, restore perfusion, strict IOs, avoid further nephrotoxins; anticipate slower recovery.
- Parameters: UOP trend, creatinine/eGFR, MAP.
Link to deeper practice sets: Med-Surg / Physiological Adaptation Case Studies and mixed-format items in the NGN Case Studies hub.
Professor’s note: If K⁺ is climbing and UOP is falling, escalate early—even if the fever just broke. Ventricular irritability trumps a “reassuring” single creatinine.
When to Worry: Red Flags & First Actions
-
Oliguria (< 0.5 mL/kg/hr) with hypotension or tachycardia
Actions: restore perfusion per protocol, stop nephrotoxins, strict IOs; evaluate for obstruction.
Parameters: MAP, UOP, mentation, creatinine. -
Fever + flank pain + systemic symptoms
Actions: cultures per policy, antibiotics per order, fluids, analgesia; monitor for sepsis.
Parameters: temperature, WOB, MAP/UOP, symptoms. -
Gross hematuria with clots or severe pain
Actions: assess obstruction/trauma; notify provider; prepare for imaging/intervention; maintain IV access.
Parameters: bleeding visibility, UOP, pain, BP. -
Rapid K⁺ rise or ECG changes in AKI
Actions: cardiac monitor; stabilize myocardium; shift/remove potassium per protocol; review meds.
Parameters: ECG, K⁺ trend, symptoms.
For electrolyte coupling, see Electrolytes Cheat Sheet (2025) and for cardiac overlap see Cardiac Markers (2025).
NGN Tie-Ins: Action → Parameter Pairs
- Pre-renal AKI (hypoperfusion) → actions: fluids/pressors per protocol, stop nephrotoxins → parameters: MAP, UOP, creatinine trend.
- Post-renal obstruction → actions: bladder scan & catheterization per order → parameters: UOP relief, pain, creatinine.
- Pyelonephritis → actions: culture then antibiotics per policy, fluids, analgesia → parameters: temperature, pain, UOP, symptoms.
- GN suspicion → actions: manage BP/edema, sodium/fluids per order, nephrotoxin review → parameters: BP, weight/edema, creatinine, UA protein/RBC trend.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
FAQs
Is a single creatinine enough to stage AKI?
No. Compare to baseline and trend with UOP, vitals, and context (volume status, nephrotoxins, obstruction).
Does a positive nitrite always mean UTI?
It increases the likelihood for certain bacteria, but interpret with symptoms and leukocyte esterase/WBCs.
What if specific gravity is fixed around 1.010?
Think poor concentrating ability (e.g., ATN). Pair with casts and the story (ischemia/nephrotoxin).
Can eGFR be “normal” in early AKI?
Yes. eGFR formulas lag; watch UOP, mentation, MAP, and repeat labs with context.