Hyperphosphatemia Nursing Care Plan (2025): CKD-MBD Made Simple, Ca×P Reality Check, and Phosphate-Binder Pearls
Study pairings: Electrolytes Cheat Sheet • Hypophosphatemia Care Plan • Calcium cluster: Hypercalcemia, Hypocalcemia
A rising serum phosphate—especially in CKD—drives CKD-MBD (mineral and bone disorder): ↓calcitriol, secondary hyperparathyroidism, bone pain/pruritus, soft-tissue/vascular calcification, and cardiac risk. For NGN, you’ll be asked to recognize the pattern, choose first-line actions (diet + phosphate binders), and build a safe monitoring plan (watch calcium, PTH, and the Ca×P conversation—useful history but not the sole driver of decisions).
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
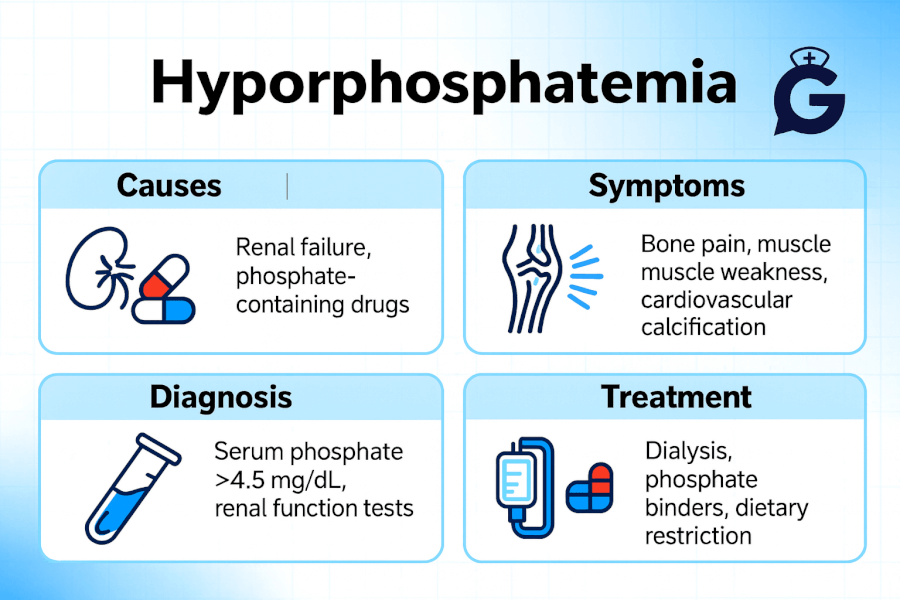
1-Minute Pattern Recognition (NGN style)
Clues: CKD/ESRD on HD/PD; pruritus; bone pain; known calcifications; recent sodium phosphate enemas/laxatives; tumor lysis syndrome (TLS); rhabdomyolysis.
Have these labs ready: Serum phosphate, total/ionized calcium, PTH, 25-OH vitamin D, creatinine/eGFR; ECG if symptomatic hypocalcemia (QT prolongation).
Compare/contrast pages:
Hyperkalemia • Hypokalemia • Hypomagnesemia • Hypermagnesemia
Pathophysiology Snapshot: CKD-MBD & the Ca×P Conversation
What’s happening?
- CKD → phosphate retention → ↑FGF23 and ↓calcitriol (1,25-OH vitamin D) → secondary hyperparathyroidism → bone turnover problems + soft-tissue/vascular calcification risk.
- Calcium–phosphate interplay: Elevated phosphate binds calcium → hypocalcemia symptoms (perioral tingling, spasms) and may raise the Ca×P product, historically tied to calcification risk.
- Modern twist: Many programs teach Ca×P (<55 mg²/dL²) as a historical check; practically, manage individual Ca²⁺ and phosphate trends—especially in CKD—rather than chasing a math product alone.
For a quick warm-up: Electrolyte Imbalances Made Easy (Mnemonics) and NGN Med-Surg Cases.
Priority Nursing Diagnoses with SMART Outcomes
1) Risk for Injury (seizure/tetany) r/t hypocalcemia secondary to hyperphosphatemia
Outcomes (24–48 h):
- No seizure/tetany; neuromuscular irritability resolved
- Ionized Ca²⁺ returns to reference range
- Patient reports early warning signs promptly (tingling, cramps)
2) Risk for Decreased Cardiac Output r/t electrolyte-induced conduction changes
Outcomes (ongoing):
- Stable rhythm on telemetry; QTc ≤ baseline
- MAP ≥ 65 mmHg without escalation of vasoactive support
3) Excess Fluid Volume / Risk for Electrolyte Imbalance r/t CKD with persistent hyperphosphatemia
Outcomes (72 h):
- Phosphate trending toward facility target range
- Dry weight stable; edema not progressing
- Dialysis adequacy goals documented if applicable
4) Deficient Knowledge (diet, binders, meds)
Outcomes (discharge):
- ≥90% teach-back accuracy on phosphate additives, binder timing with meals, OTC laxatives to avoid, and follow-up labs
Interventions & Rationales (What to do, Why it works)
Safety First: Cardiac + Neuro
- Place on telemetry if symptomatic; institute seizure precautions.
Rationale: Hyperphosphatemia can cause hypocalcemia → arrhythmias/seizure risk. - Reserve IV calcium for symptomatic hypocalcemia (tetany, seizures, dangerous QT); in severe phosphate elevation (e.g., TLS), indiscriminate calcium may worsen Ca-phosphate precipitation.
External resource: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/tumor-lysis-syndrome
Confirm Persistence → Treat
- Trend phosphate (don’t overreact to one blip). If persistently elevated, initiate binder/diet changes; avoid routine binders when phosphate is normal.
External resource: https://kdigo.org/guidelines/ckd-mbd/
Binder Strategy (with meals)
- Calcium-free options: sevelamer, lanthanum, ferric citrate—useful when avoiding extra calcium load or with calcification risk.
- Restrict calcium-based binders (calcium acetate/carbonate) if hypercalcemia or calcification concerns.
- Avoid chronic aluminum binders.
Teaching hook: “Binders with bites”—timing alongside meals/snacks maximizes binding.
Diet: Target the Absorbable Sources
- Limit “phos-” additives (processed foods, shelf-stable meats, flavored drinks).
- Prefer fresh foods; coordinate protein targets with renal diet stage.
External resource: https://www.niddk.nih.gov/health-information/kidney-disease/mineral-bone-disorder
Dialysis Optimization
- For patients on HD/PD, collaborate to increase dialytic phosphate removal if levels remain high despite diet/binders.
- In TLS or severe AKI with life-threatening electrolytes, hemodialysis may be required (nephrology/oncology driven).
Absolute Caution with Sodium Phosphate OTCs
- Avoid sodium phosphate enemas/purgatives in CKD unless specifically directed; never exceed labeled doses.
External resource: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-over-the-counter-sodium-phosphate-products
Build judgment range: ABG Cases—15 practice • NGN Pharmacology Cases • How to Read NGN Case Stems
Binder Mini-Cheat Sheet (clinicals & NCLEX)
| Scenario | Likely First-Line Considerations | Nursing Notes |
|---|---|---|
| CKD with persistent high phosphate, normal calcium | Sevelamer or lanthanum | Take with meals; watch GI upset; reinforce label reading for additives |
| CKD with hypercalcemia or calcification risk | Prefer calcium-free binders | Avoid extra calcium load; trend Ca²⁺ and phosphate together |
| Iron deficiency + high phosphate | Ferric citrate (binder + iron) per provider | Monitor ferritin/TSAT per protocol |
| Severe, refractory elevation on dialysis | Increase dialytic removal | Coordinate with nephrology; reassess diet/binder adherence |
Calcium decisions often run alongside PTH/Vit D decisions—review Hypocalcemia and Primary Hyperparathyroidism.
Patient Teaching (Stick-to-the-fridge Bullets)
- Labels matter: Avoid foods with “phos-” in the ingredients.
- Binders = with bites: Take your phosphate binder with every meal/snack.
- Call us for: new muscle cramps, tingling around lips/fingers, palpitations, chest pain.
- OTC alert: No sodium phosphate enemas/laxatives unless your kidney team says so.
- Keep labs: come to scheduled blood tests—this is how we adjust your plan safely.
Documentation Tips (NGN-ready)
- Record trend (not just a single phosphate).
- Note binder name, dose, and timing with meals.
- Include dietary counseling provided and patient teach-back success.
- If dialysis, document removal strategy changes and nephrology coordination.
- Add safety line: “Patient instructed to avoid OTC sodium phosphate products.”
FAQ (PAA-Style)
What phosphate level is “high” and when do we treat?
Most labs cite ~2.5–4.5 mg/dL as normal. In CKD, act when phosphate is persistently or progressively elevated (not a one-off). Treatment intensity depends on symptoms, calcium, PTH, and overall risk profile.
Do we still use the Ca×P product?
Know the historical <55 mg²/dL² teaching—but in practice, manage based on individual calcium and phosphate levels/trends and clinical risk (calcifications, symptoms, stage of CKD).
Which binders are calcium-free?
Sevelamer, lanthanum, ferric citrate. Reserve or limit calcium-based binders when hypercalcemia or calcification risk exists.
Can I give IV calcium if the patient is hypocalcemic?
Give only for symptomatic hypocalcemia (tetany, seizures, dangerous QT). In severe hyperphosphatemia (e.g., TLS), indiscriminate calcium can precipitate with phosphate; prioritize lowering phosphate.
When is dialysis indicated for hyperphosphatemia?
If phosphate remains high despite diet + binders in dialysis patients, collaborate to increase removal. In TLS or severe AKI, dialysis may be required to rapidly control life-threatening electrolyte derangements.
GoodNurse: Keep Going (Cross-Links)
-
Study hubs:
-
Electrolyte care plans:
References
- KDIGO. Clinical Practice Guideline Update for CKD–MBD (2017). Available at: https://kdigo.org/guidelines/ckd-mbd/
- NIDDK (NIH). Mineral & Bone Disorder in Chronic Kidney Disease. Available at: https://www.niddk.nih.gov/health-information/kidney-disease/mineral-bone-disorder
- U.S. FDA. Drug Safety Communication: Risks from over-the-counter sodium phosphate products. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-over-the-counter-sodium-phosphate-products
- National Cancer Institute. Tumor Lysis Syndrome (Dictionary of Cancer Terms). Available at: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/tumor-lysis-syndrome