When deep tendon reflexes fade and the blood pressure drifts low on a magnesium infusion, you need a clear plan—fast. In clinicals and precepting, I’ve seen hypermagnesemia sneak up during obstetric MgSO₄ therapy and in patients with kidney failure taking OTC antacids or laxatives. This NGN-ready guide gives you a calm, stepwise approach: quick pathophysiology, priority nursing diagnoses with SMART outcomes, and interventions with rationales—centered on recognizing toxicity, administering IV calcium to antagonize magnesium, supporting airway and breathing, and removing excess Mg²⁺ with diuretics or dialysis as ordered.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Pathophysiology of Hypermagnesemia
Hypermagnesemia typically arises when intake exceeds excretion, most often in acute or chronic kidney disease (reduced renal clearance) or during/after therapeutic magnesium sulfate infusions (e.g., preeclampsia/eclampsia). Other contributors include Mg-containing antacids/laxatives, total parenteral nutrition, and tumor lysis or massive cell breakdown. Magnesium acts as a physiologic calcium-channel antagonist and neuromuscular depressant; rising serum Mg²⁺ produces a dose-related progression:
- Mild–moderate: flushing, warmth, nausea, hypotension, bradycardia, diminished deep tendon reflexes (DTRs)
- Severe: somnolence, respiratory depression, heart block, cardiac arrest
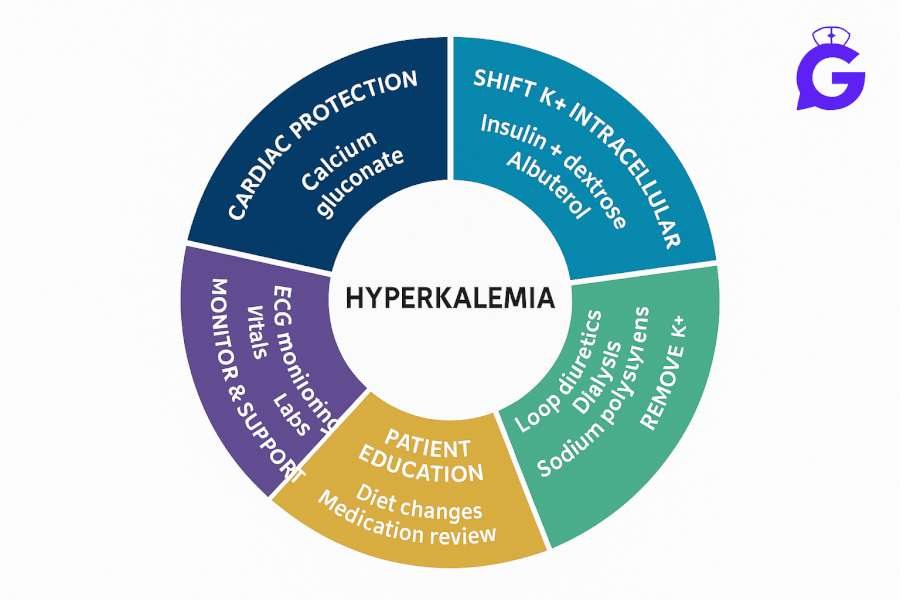
Core management pillars are: 1) stop exogenous magnesium, 2) stabilize with IV calcium (antagonizes Mg²⁺ at the neuromuscular junction and myocardium), 3) support ventilation and hemodynamics, and 4) enhance elimination (loop diuretics with IV fluids if kidneys work; hemodialysis when they don’t).
Cross-reference related electrolyte plans for rapid differentials and teaching: Hypomagnesemia, Hyperkalemia, Hypokalemia, Hypernatremia, and the calcium cluster: Hypercalcemia, Hypocalcemia, Primary Hyperparathyroidism, Hypercalcemia of Malignancy, Calcium Kidney Stones. Study helpers: Electrolyte Imbalances Made Easy, Electrolytes Cheat Sheet, ABG Interpretation, NGN Med-Surg Case Studies.
Nursing Care Plans for Hypermagnesemia
Below are NGN-style diagnoses with SMART outcomes and interventions/rationales. Individualize to orders and facility protocol.
Nursing Diagnosis: Risk for Ineffective Breathing Pattern (respiratory depression)
| Category | Details |
|---|---|
| Related to | Neuromuscular depression from elevated serum magnesium |
| As evidenced by | Diminished DTRs, somnolence, shallow respirations, hypoventilation, rising CO₂ (if available) |
| Desired Outcomes | RR 12–20/min with adequate tidal volume; SpO₂ ≥ 94% on ordered O₂; no escalation to ventilatory support. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Place on continuous pulse oximetry; assess work of breathing and level of sedation frequently. | Early detection of hypoventilation enables timely airway support. |
| Stop exogenous magnesium (infusions, antacids/laxatives) and notify provider promptly. | Removes ongoing source to prevent worsening toxicity. |
| Administer IV calcium (e.g., calcium gluconate) per order for symptomatic toxicity. | Physiologically antagonizes magnesium at the heart and neuromuscular junction to improve contraction and respiratory drive. |
Nursing Diagnosis: Risk for Decreased Cardiac Output (bradycardia/heart block)
| Category | Details |
|---|---|
| Related to | AV nodal depression and vasodilation from hypermagnesemia |
| As evidenced by | Hypotension, bradycardia, prolonged PR/QRS, heart block; dizziness or syncope |
| Desired Outcomes | MAP ≥ 65 mmHg; HR within ordered parameters; stable rhythm without high-grade block. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Initiate continuous cardiac monitoring; obtain baseline and follow-up 12-lead ECGs. | Detects conduction delays/blocks and trends response to therapy. |
| Maintain IV access; prepare vasoactive support per protocol if hypotension persists. | Ensures rapid intervention for hemodynamic instability. |
| Administer ordered IV calcium; escalate to pacing/advanced interventions per ACLS if indicated. | Calcium counters magnesium’s cardiac effects while definitive elimination proceeds. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Excess Fluid Volume or Risk for Electrolyte Imbalance (renal failure/ongoing Mg load)
| Category | Details |
|---|---|
| Related to | Decreased renal clearance of magnesium; ongoing OTC Mg antacids/laxatives; TPN |
| As evidenced by | Rising Mg²⁺ levels; edema; reduced urine output; CKD/AKI on history |
| Desired Outcomes | Serum Mg²⁺ returns to target; no rebound after source removal; stable fluid status. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Verify and hold Mg-containing meds/supplements; perform medication reconciliation (OTC antacids, laxatives). | Prevents re-loading while treatment proceeds. |
| Promote elimination: administer loop diuretic with IV fluids if renal function adequate; prepare for dialysis if ordered. | Enhances magnesium clearance; dialysis rapidly removes Mg²⁺ in renal failure. |
| Trend Mg²⁺, K⁺, Ca²⁺; monitor DTRs, level of consciousness, and urine output. | Tracks progression/resolution and detects complications early. |
Nursing Diagnosis: Deficient Knowledge (toxicity signs & prevention)
| Category | Details |
|---|---|
| Related to | Unfamiliarity with safe Mg use in CKD and with obstetric infusions |
| As evidenced by | Questions about OTC products, monitoring DTRs/respirations, and when to seek care |
| Desired Outcomes | Patient/family teach back early toxicity signs and medication safety; avoids Mg-containing OTCs unless cleared by provider. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach red-flag symptoms: progressive somnolence, muscle weakness, slowed breathing, loss of DTRs, bradycardia. | Promotes early escalation for worsening toxicity. |
| In CKD, avoid Mg-containing OTCs unless prescribed; review labels for “magnesium hydroxide/carbonate.” | Prevents inadvertent re-exposure in reduced clearance states. |
| For obstetric MgSO₄ infusions, reinforce monitoring plan: DTRs, RR, urine output; when to notify RN/provider. | Standardizes safety during therapeutic use and catches early toxicity. |
NGN Clinical Judgment Pearls
- DTRs are your canary: diminishing reflexes often precede respiratory depression—trend and document clearly.
- Calcium is the antidote: IV calcium reverses acute effects but doesn’t remove magnesium—always pair with elimination strategies.
- Think kidneys and OTCs: in CKD, even “harmless” antacids/laxatives can cause severe hypermagnesemia.
- Co-electrolytes matter: follow K⁺ and Ca²⁺; bradyarrhythmias or heart block may require ACLS-guided escalation.
Frequently Asked Questions (FAQ)
What are early signs of magnesium toxicity during MgSO₄ therapy?
Flushing/warmth, nausea, hypotension, diminished DTRs, and increasing somnolence. Escalate if RR slows or patient becomes difficult to arouse.
Why give IV calcium in hypermagnesemia?
Calcium physiologically antagonizes magnesium’s effects on the heart and neuromuscular junction, improving contractility and respiratory drive while you remove excess Mg²⁺.
How is magnesium removed from the body when kidneys are impaired?
Hemodialysis rapidly clears magnesium and is indicated for severe toxicity with renal failure. If renal function is intact, loop diuretics with IV fluids can enhance excretion.
Which patients are at highest risk?
Those with CKD/AKI using Mg-containing OTCs, patients on prolonged MgSO₄ infusions, older adults, and individuals receiving TPN or certain chemotherapies.
Further Reading
- Hypomagnesemia Nursing Care Plan
- Hyperkalemia Nursing Care Plan
- Hypokalemia Nursing Care Plan
- Hypernatremia Nursing Care Plan
- Hypercalcemia Nursing Care Plan
- Hypocalcemia Nursing Care Plan
- Primary Hyperparathyroidism Nursing Care Plan
- Hypercalcemia of Malignancy Nursing Care Plan
- Calcium Kidney Stones (Nephrolithiasis) Nursing Care Plan
- Electrolyte Imbalances Made Easy: Mnemonics
- Electrolytes Cheat Sheet (Na⁺/K⁺/Ca²⁺/Mg²⁺ Patterns)
- ABG Interpretation: 15 Practice Cases
- NGN Med-Surg Case Studies