When calcium is high and the clues point to the parathyroids, students often ask: “Where do I even start?” I’ve taught this countless times at the bedside—primary hyperparathyroidism (PHPT) can look subtle (fatigue, kidney stones, bone pain) or present as true hypercalcemia emergencies. In this NGN-ready guide, I’ll show you a clear, exam-and-clinical path: quick pathophysiology, prioritized nursing diagnoses with SMART outcomes, and specific interventions with rationales. You’ll know what to assess first, how to prevent complications (stones, bones, groans), and how to teach patients in plain language—especially those headed to endocrine surgery.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- Pathophysiology of Primary Hyperparathyroidism
- Nursing Care Plans (Diagnoses, Outcomes, Interventions & Rationales)
- FAQs
- Further Reading
- References
Pathophysiology of Primary Hyperparathyroidism
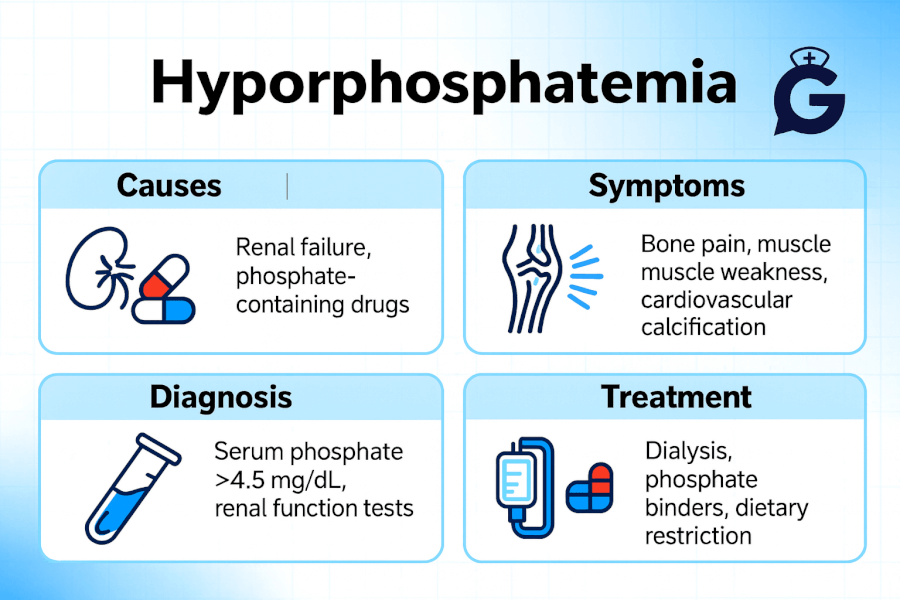
Primary hyperparathyroidism is an endocrine disorder in which one or more parathyroid glands autonomously secrete excess parathyroid hormone (PTH), most often due to a solitary adenoma. Elevated PTH increases bone resorption, renal calcium reabsorption, and activation of vitamin D, leading to hypercalcemia and hypophosphatemia. Patients may be asymptomatic or show the classic “stones, bones, abdominal groans, and psychic overtones” from chronic calcium elevation. Diagnosis typically includes elevated calcium with inappropriately high PTH; imaging is pre-operative localization, not diagnostic. Definite treatment is parathyroidectomy when criteria are met; otherwise, medical management focuses on hydration, activity, and monitoring (NIDDK/NIH; Endocrine Society).
Master the calcium differential by pairing this with its clinical counterparts:
• Hypercalcemia Nursing Care Plan (2025)
• Hypocalcemia Nursing Care Plan (2025)
Build clinical reasoning with ABG Interpretation: 15 Practice Cases and NGN judgment with NGN Med-Surg Physiological Adaptation.
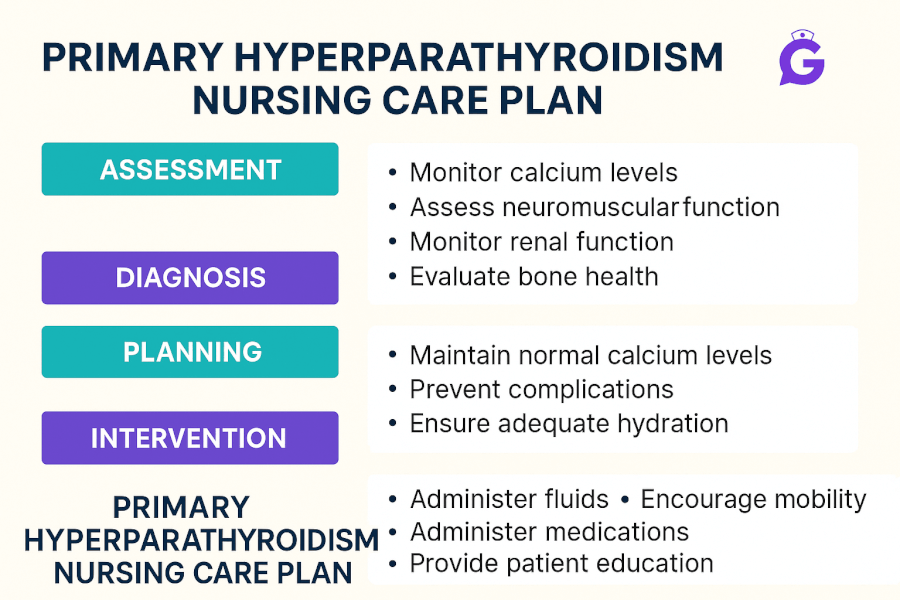
Nursing Care Plans for Primary Hyperparathyroidism
Use these NGN-style diagnoses, outcomes, and interventions to individualize care. Many priorities mirror hypercalcemia management while you coordinate endocrine/surgical care.
Nursing Diagnosis: Risk for Deficient Fluid Volume
| Category | Details |
|---|---|
| Related to | Osmotic diuresis from hypercalcemia causing polyuria and dehydration |
| As evidenced by | (Risk factors) Elevated serum calcium, increased urine output, low urine specific gravity, thirst, dry mucosa |
| Desired Outcomes | Maintain MAP > 65 mmHg, UO ≥ 0.5–1 mL/kg/hr, stable weight, improved turgor; labs trend toward normal calcium per provider targets within 24–48 hrs. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Initiate/monitor isotonic IV fluids per order; strict I&O; daily weights. | Volume repletion enhances renal calcium excretion and prevents prerenal AKI. |
| Review medications (thiazides, calcium/vitamin D supplements) and collaborate on adjustments. | These agents can worsen hypercalcemia in PHPT. |
| Teach oral hydration targets and schedule reminders. | Sustained hydration reduces stone risk and corrects volume deficit. |
Nursing Diagnosis: Risk for Renal Calculi
| Category | Details |
|---|---|
| Related to | Chronic hypercalciuria from elevated PTH; dehydration; reduced activity |
| As evidenced by | (Risk factors) History of nephrolithiasis, flank pain, hematuria, elevated urine calcium |
| Desired Outcomes | No flank pain/hematuria; UO adequate; patient demonstrates stone-prevention strategies before discharge. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Strain urine if stones suspected; monitor for hematuria and escalating flank pain. | Early detection guides urology referral and prevents obstruction/AKI. |
| Encourage mobility and ROM exercises. | Activity reduces bone resorption and urinary calcium losses. |
| Provide diet education: maintain normal dietary calcium, avoid excessive supplements; review sodium/oxalate moderation if advised. | Balanced intake and hydration lower stone risk more effectively than severe restriction. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Risk for Injury (bone loss/pathologic fracture)
| Category | Details |
|---|---|
| Related to | PTH-mediated cortical bone loss; muscle weakness and balance changes from hypercalcemia |
| As evidenced by | (Risk factors) Low BMD on DXA, history of fractures, gait instability, age > 50 |
| Desired Outcomes | Remains free from falls; demonstrates home safety plan; participates in weight-bearing/strength training per tolerance. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Implement fall precautions; assess gait; coordinate PT/OT if indicated. | Prevents falls and fractures during periods of weakness or confusion. |
| Reinforce weight-bearing exercise program and smoking/alcohol moderation. | Supports bone density and reduces fracture risk. |
Nursing Diagnosis: Deficient Knowledge (disease, surgery, post-op care)
| Category | Details |
|---|---|
| Related to | Unfamiliarity with PHPT, indications for parathyroidectomy, and post-op hypocalcemia monitoring |
| As evidenced by | Questions about surgery, incision care, medications/supplements, and stone prevention |
| Desired Outcomes | Patient/family teach back the plan: hydration, activity, medication adjustments, post-op signs of hypocalcemia (tingling, cramps, hoarseness/stridor) and when to seek care. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach hydration goals, urine monitoring, and avoiding unnecessary calcium/vitamin D supplements unless prescribed. | Prevents stones and recurrent hypercalcemia from over-supplementation. |
| Review parathyroidectomy expectations and **post-op hypocalcemia** surveillance; keep calcium gluconate available per protocol. | Transient hypocalcemia may occur post-op due to “hungry bone” syndrome; early recognition prevents airway/cardiac complications. |
| Provide written return precautions: worsening confusion, severe constipation, palpitations, flank pain, peri-oral tingling, hoarseness/stridor. | Supports timely escalation for cardiac, renal, or airway issues. |
Frequently Asked Questions (FAQ)
What is the priority nursing intervention for primary hyperparathyroidism with hypercalcemia?
Safety and aggressive hydration with isotonic IV fluids as prescribed. Hydration improves renal calcium excretion; simultaneously address reversible contributors (e.g., hold thiazides and unnecessary calcium/vitamin D).
When is parathyroid surgery indicated?
Indications include symptoms (stones, fractures), very high calcium, reduced kidney function, osteoporosis/low BMD, or age criteria—determined by endocrinology/surgery guidelines (Endocrine Society).
Why do patients form kidney stones in PHPT?
Excess PTH increases calcium release from bone and renal reabsorption, leading to hypercalciuria; dehydration concentrates urine, crystallizing calcium-based stones.
What is “hungry bone” syndrome after parathyroidectomy?
After removal of the overactive gland, bone avidly takes up calcium/phosphate, causing transient hypocalcemia; monitor for tetany/tingling and replace calcium/magnesium as ordered.
Which medications should be reviewed in PHPT?
Thiazide diuretics and calcium/vitamin D supplements can raise calcium levels; evaluate risks/benefits with the provider. In malignancy-related hypercalcemia, agents like bisphosphonates/denosumab may be used under specialist guidance.
Further Reading
- Hypercalcemia Nursing Care Plan (2025)
- Hypocalcemia Nursing Care Plan (2025)
- ABG Interpretation: 15 Practice Cases (with Rationale)
- NGN Med-Surg Case Studies: Physiological Adaptation
- NGN Pharmacology Case Studies: 10 Examples with Answers