When a medication has a narrow therapeutic window, you’re not just giving a dose—you’re managing risk vs benefit in real time. This guide focuses on three high-yield drugs for nursing practice and NGN reasoning: vancomycin, digoxin, and lithium. You’ll see when to draw levels, how to read them in clinical context, and what to do first when the picture points toward toxicity.
If you want full lab ranges at your elbow, keep Normal Lab Values (2025): Printable Cheat Sheet nearby. For acid–base and perfusion context that often coexists with drug issues, pair this with ABG Interpretation Made Simple (2025). To reset your approach on crowded stems, use How to Read NGN Case Stems (2025).
Table of Contents
- Why Therapeutic Drug Monitoring (TDM) Matters
- Quick Reference Table
- Vancomycin: Timing, Targets, Toxicity, Teaching
- Digoxin: Timing, Targets, Toxicity, Teaching
- Lithium: Timing, Targets, Toxicity, Teaching
- When to Worry: Red Flags & First Actions
- NGN Tie-Ins: Action → Parameter
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Why Therapeutic Drug Monitoring (TDM) Matters
- Goal: Maintain efficacy while avoiding toxicity.
- Reality: Levels are data points, not verdicts. They make sense only with symptoms, vitals, renal/hepatic function, and timing of the draw.
- Nursing edge: You control when the sample is drawn, what you assess around it, and how quickly you act on red flags.
Professor’s note: Before you look at a level, ask: “What problem am I treating and what parameter should change first?” That habit guides safe dosing and NGN points.
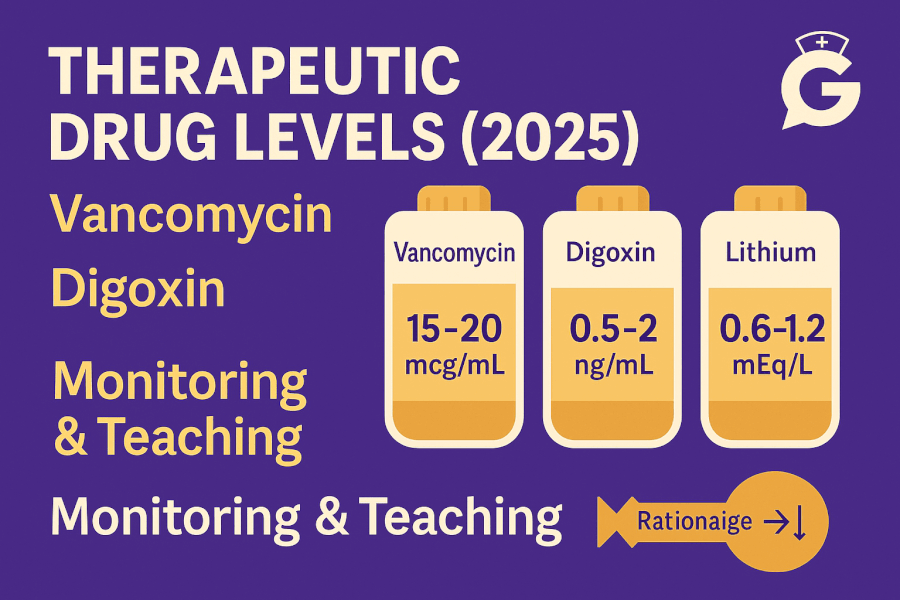
Quick Reference Table
Use this as a memory jogger. Always follow your facility’s protocol and lab reference intervals.
| Drug | Typical Draw Timing | Practical Targets* | Key Toxicity Signs | Nurse Priorities |
|---|---|---|---|---|
| Vancomycin | Trough at steady state (often before 4th dose) Many sites use AUC-based monitoring |
Troughs often ~10–15 mg/L (mild) or 15–20 mg/L (serious infections) or AUC/MIC per protocol |
Rising creatinine (AKI), ototoxicity (rare), infusion reaction (red-man) | Check renal trends, IOs, infusion rate; verify timing for accurate draws; report AKI signs promptly |
| Digoxin | At least 6–8 h post-dose (many draw ~8–12 h) and at steady state | ~0.5–0.9 ng/mL (HF goals often at lower end; follow local targets) | GI upset, confusion, visual changes (yellow/green), bradyarrhythmias | Check K⁺/Mg²⁺, apical pulse, ECG; hold for brady per orders; anticipate digoxin-Fab in severe toxicity |
| Lithium | Trough ~12 h after last dose; steady state after several days | Maintenance commonly ~0.6–1.0 mEq/L (local ranges vary) | Tremor, GI upset, ataxia, confusion; severe: seizures, coma | Assess hydration, Na⁺ intake, renal/thyroid trends; watch for interacting meds (NSAIDs, diuretics) |
*Targets and intervals vary—always confirm with your facility’s policies and the prescriber’s plan.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Vancomycin: Timing, Targets, Toxicity, Teaching
Why monitor? Efficacy vs nephrotoxicity. Many institutions now emphasize AUC-based assessment (overall exposure) rather than single troughs alone. On the floor you’ll still see trough draws and dose adjustments guided by pharmacy.
Timing
- Draw just before the next dose at steady state (often before the 4th dose) unless your site uses a different schedule or AUC-based sampling.
- Document exact times of dose administration and sample collection—off-by-one-hour draws can mislead.
Interpreting levels
- Troughs around 10–15 mg/L are common for less severe infections; 15–20 mg/L may be used in serious infections—follow local protocol.
- If AUC monitoring is in place, expect pharmacy to request two appropriately timed levels or use Bayesian software. Your job: accurate timing and complete charting.
Nursing actions
- Monitor creatinine/eGFR and urine output; rising creatinine or oliguria can signal AKI risk.
- Infuse at recommended rates to reduce infusion reactions. If flushing/pruritus occurs (red-man syndrome), slow/hold per protocol and notify the provider.
- Maintain hydration as ordered; avoid nephrotoxins when possible (e.g., NSAIDs).
- Coordinate with pharmacy on dose adjustments and re-draw timing.
Teaching points for clients
- Report ringing in ears, decreased urine, or severe rash.
- Keep lab appointments on time; dosing may change based on results.
For kidney context and red flags, see Renal Function & UA Interpretation (2025).
Digoxin: Timing, Targets, Toxicity, Teaching
Why monitor? Narrow therapeutic index and strong link to electrolytes, especially potassium. Hypokalemia makes myocardium more sensitive to digoxin, raising toxicity risk.
Timing
- Draw levels at least 6–8 hours after the last dose (many protocols use 8–12 hours) and only after steady state is reached.
- Document last dose time—early draws can overestimate the steady-state concentration.
Interpreting levels
- Many HF protocols aim for ~0.5–0.9 ng/mL (lower end minimizes toxicity); other indications may differ. Always follow your site’s targets.
- Symptoms trump numbers—mildly “therapeutic” values can still be toxic if potassium is low or if the client is symptomatic.
Toxicity watch
- GI: anorexia, nausea, vomiting.
- Neuro/visual: fatigue, confusion, yellow/green halos.
- Cardiac: bradycardia, AV block, arrhythmias (monitor ECG).
- Risk rises with hypokalemia/hypomagnesemia (diuretics), renal impairment, drug interactions.
Nursing actions
- Check apical pulse per order; hold for bradycardia as specified.
- Review K⁺/Mg²⁺ and correct abnormalities (see Electrolytes (2025)).
- If toxicity suspected: place on ECG monitor, notify provider, anticipate digoxin-specific Fab in severe cases, and address potassium carefully based on rhythm and renal function.
Teaching points for clients
- Take at the same time daily; don’t double doses if you forget—call the clinic.
- Report nausea, vision changes, dizziness, palpitations.
- Keep potassium in the target range per provider; ask before starting new meds.
Lithium: Timing, Targets, Toxicity, Teaching
Why monitor? Very narrow therapeutic window; levels rise with dehydration, low sodium, and interactions (e.g., NSAIDs, thiazide diuretics). Although lithium is psychiatric, nurses frequently manage fluids, labs, and safety across settings.
Timing
- Draw trough levels ~12 hours after the last dose (morning draw after evening dose is common).
- Wait until steady state (several days) for maintenance checks or sooner if symptoms suggest toxicity.
Interpreting levels
- Maintenance targets vary; many aim for ~0.6–1.0 mEq/L (follow local guidance and prescriber plan).
- Toxicity often starts >1.5 mEq/L, but symptoms at lower levels can occur with dehydration or comorbid illness.
Toxicity watch
- Early: fine tremor, thirst, polyuria, GI upset.
- Progressing: coarse tremor, ataxia, confusion, slurred speech.
- Severe: seizures, arrhythmias, coma—medical emergency.
Nursing actions
- Assess hydration, sodium intake, and renal function; dehydration elevates levels.
- Clarify use of NSAIDs/diuretics—both can raise lithium.
- If toxicity suspected: hold dose, obtain level, manage fluids per order, implement safety (fall/seizure precautions), and escalate rapidly for severe symptoms.
Teaching points for clients
- Maintain consistent salt and fluid intake; avoid dehydration (fever, exercise, heat).
- Check before adding OTCs like ibuprofen or naproxen.
- Expect periodic checks of kidney and thyroid function.
When to Worry: Red Flags & First Actions
-
Vancomycin + rising creatinine or oliguria
Actions: review timing and doses, notify provider/pharmacy, hold/adjust per order; ensure accurate timing for any repeat levels; monitor IOs and MAP.
Parameters: creatinine/eGFR, UOP, symptoms, trough/AUC follow-up. -
Digoxin + bradyarrhythmia with visual changes
Actions: place on ECG monitor; follow hold parameters; check K⁺/Mg²⁺; anticipate digoxin-Fab per order in severe cases.
Parameters: HR/rhythm, K⁺/Mg²⁺, symptoms. -
Lithium + ataxia/confusion or coarse tremor
Actions: hold dose, obtain stat lithium level and BMP; support hydration; review meds for interactions; implement safety.
Parameters: lithium level, mentation, gait, Na⁺, creatinine.
For integrated patterns (renal injury affecting multiple drugs), see Renal Function & UA Interpretation (2025) and Coagulation Studies (2025) for procedures and bleeding risk considerations.
NGN Tie-Ins: Action → Parameter
- Vancomycin nephrotoxicity → actions: adjust/hold per order, optimize hydration, avoid nephrotoxins → parameters: creatinine/eGFR, UOP.
- Digoxin with hypokalemia → actions: correct K⁺, ECG monitor, evaluate for Fab → parameters: ECG rhythm, K⁺ trend, symptoms.
- Lithium with dehydration → actions: hold dose, rehydrate per order, check interactions → parameters: lithium level, mentation, Na⁺, creatinine.
Professor’s note: Pick parameters that move soon: HR/rhythm for digoxin, UOP/Cr for vancomycin AKI risk, mentation/ataxia for lithium. That’s how you “prove it worked” on NGN—and at the bedside.
FAQs
Do levels alone prove toxicity?
No. Levels are supportive. Symptoms and context decide urgency and treatment.
Why is my digoxin level “therapeutic,” but the client looks toxic?
Electrolytes, renal function, and timing of the draw can mislead. Treat the client—not just the number.
Is AUC monitoring for vancomycin better than troughs?
Many sites are moving that way. Your role is accurate timing, excellent documentation, and quick reporting of renal changes.
Why does dehydration raise lithium levels?
Lithium tracks with sodium and water balance. Low sodium or volume depletion reduces excretion, raising levels.
What should I chart with every level?
Time of last dose, time of draw, pertinent vitals/symptoms, recent fluid balance, and any new meds.