When bleeding or clotting is on the table, minutes matter. This cheat sheet compresses PT/INR, aPTT, fibrinogen, and D-dimer into quick ranges, interpretation patterns, and nurse-priority actions you can apply in clinicals and on NGN items.
Keep the full ranges nearby with Normal Lab Values (2025): Printable Cheat Sheet. If a stem mixes coag labs with oxygenation/perfusion issues, pair this with ABG Interpretation Made Simple (2025). When a case stem feels crowded, reset with How to Read NGN Case Stems (2025).
Table of Contents
- How to Use This Cheat Sheet
- Quick Reference Ranges
- PT/INR
- aPTT
- Fibrinogen
- D-dimer
- Anticoagulant Monitoring & Reversal
- When to Worry: Red Flags & First Actions
- NGN Tie-Ins: Action → Parameter Pairs
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
How to Use This Cheat Sheet
- Name the single priority (bleeding risk vs thrombosis risk vs consumptive coagulopathy).
- Choose two actions that change physiology now (pressure, product replacement, anticoagulant hold/reversal, oxygenation).
- Pick two parameters to reassess soon (Hgb/VS/bleeding, mental status, INR/aPTT/fibrinogen trend).
- Remember: lab ranges and therapeutic targets vary by facility and indication—confirm locally.
Professor’s note: If two answers seem reasonable, pick the pair that controls hemorrhage or halts clot propagation fastest—and choose parameters that prove it worked within minutes to hours.
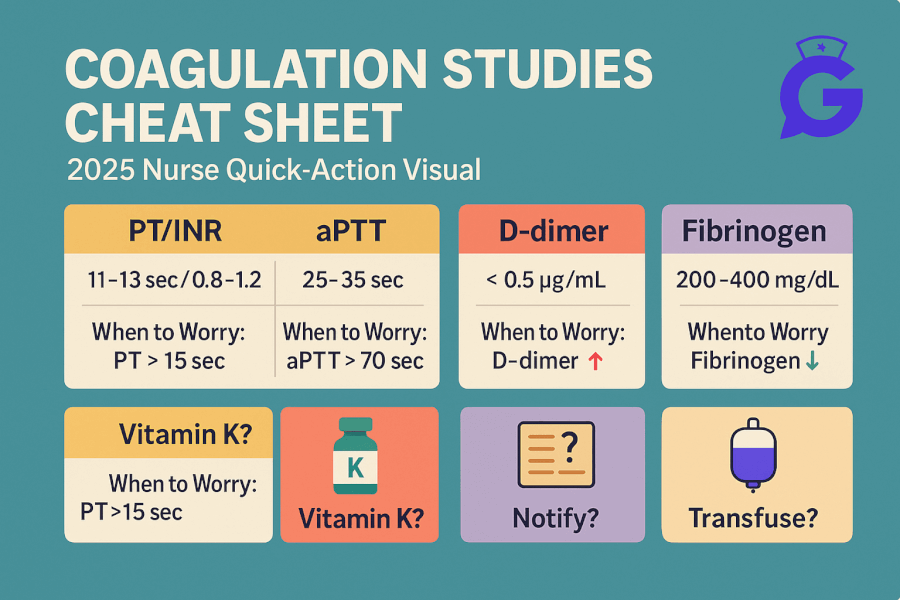
Quick Reference Ranges
| Test | Typical Adult Reference* | What it tells you |
|---|---|---|
| PT | ~11–13.5 s | Extrinsic/common pathway; prolonged in warfarin effect, liver disease, DIC |
| INR | ~0.8–1.2 (non-anticoagulated) | Standardized PT; target range depends on indication (e.g., 2.0–3.0 common) |
| aPTT | ~25–35 s | Intrinsic/common pathway; prolonged in unfractionated heparin, severe factor deficiencies, DIC |
| Fibrinogen | ~200–400 mg/dL | Substrate for clot formation; low in DIC, severe liver disease, massive bleeding |
| D-dimer | Negative/low per lab cutoff | Fibrin degradation product; elevated with clot formation/lysis (PE/DVT workups, DIC) |
*Always use your facility’s reference intervals and therapeutic targets.
PT/INR
What it reflects: Function of the extrinsic pathway (factor VII) and common pathway (X, V, II, fibrinogen).
Why it matters: Monitoring warfarin effect; prolonged in vitamin K deficiency, liver dysfunction, DIC, massive transfusion.
Interpretation patterns
- Elevated INR on warfarin with bleeding → hold warfarin; consider vitamin K and reversal strategies per protocol.
- Elevated INR without warfarin → think liver disease, vitamin K deficiency (malnutrition/antibiotics), or DIC (check platelets, fibrinogen, D-dimer).
- Therapeutic range is indication-specific (e.g., atrial fibrillation vs mechanical valves).
aPTT
What it reflects: Intrinsic and common pathways (VIII, IX, XI, XII; X, V, II, fibrinogen).
Why it matters: Monitoring unfractionated heparin; prolonged in severe factor deficiencies, DIC, lupus anticoagulant.
Interpretation patterns
- Prolonged aPTT on heparin infusion → adjust per nomogram; reassess bleeding and aPTT per schedule.
- Prolonged aPTT with normal PT in a non-heparinized client → consider intrinsic factor issues or inhibitors; check history (hemophilia, acquired inhibitors).
- If both PT/INR and aPTT are prolonged → think DIC, severe liver disease, or massive transfusion coagulopathy.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Fibrinogen
What it reflects: Final substrate converted to fibrin; consumed in DIC and depleted with massive hemorrhage.
Nursing implications: Low fibrinogen can mean poor clot stability—watch for oozing from lines, mucosal bleeding.
Interpretation patterns
- Low fibrinogen + prolonged PT/aPTT + thrombocytopenia + high D-dimer → DIC pattern.
- Massive transfusion → dilutional coagulopathy; fibrinogen may fall and require cryoprecipitate per protocol.
D-dimer
What it reflects: Fibrin degradation after clot formation; very sensitive but not specific.
Use case: Helps rule out PE/DVT in low/moderate pretest probability when negative; positive needs context (inflammation, infection, pregnancy, post-op can elevate).
Nursing tips
- Don’t over-interpret a positive D-dimer alone; pair with exam, imaging, and risk tools.
- Track clinical course: oxygenation, WOB, hemodynamics if PE is suspected—labs don’t replace assessment.
Anticoagulant Monitoring & Reversal
| Drug/Class | Primary Monitor | Key Notes | Reversal/Countermeasures* |
|---|---|---|---|
| Warfarin | INR | Diet/drug interactions; slow onset/offset | Vitamin K; PCC/FFP per protocol & severity |
| Unfractionated Heparin (UFH) | aPTT (or anti-Xa per protocol) | Short half-life; nomogram-guided titration | Protamine sulfate (dose per recent units) |
| LMWH (e.g., enoxaparin) | Anti-Xa (selected cases) | Renal dosing; predictable PK | Partial reversal with protamine (variable) |
| DOACs (e.g., apixaban, rivaroxaban, dabigatran) | No routine lab; specialized assays may exist | Renal/hepatic considerations; fewer food interactions | Agent-specific reversal where available; supportive care per protocol |
*Follow institutional protocols and formulary for reversal agents and dosing.
Professor’s note: In hemorrhage, two questions matter first: Can you control the bleeding now? and What product reverses the physiology? Pick parameters that move fast—visible bleeding, MAP, mental status, and lab trends.
When to Worry: Red Flags & First Actions
-
Visible bleeding with elevated INR (warfarin)
Actions: hold warfarin; consider vitamin K and reversal products per protocol; apply pressure; secure IV access.
Parameters: visible bleeding, Hgb/Hct, INR, MAP/mentation. -
Oozing from lines, low fibrinogen, prolonged PT/aPTT, thrombocytopenia
Actions: treat cause; anticipate product support (cryoprecipitate/FFP/platelets) per order; check temperature and calcium during massive transfusion.
Parameters: fibrinogen, clotting time trend, temperature, ionized Ca²⁺, MAP. -
PE/DVT suspicion with positive D-dimer and hypoxemia
Actions: oxygen to target sats; rapid diagnostic pathway; anticoagulation per order if confirmed and safe.
Parameters: SpO₂/WOB, hemodynamics, symptom trajectory; see ABG Interpretation for gas exchange context. -
Excess anticoagulation on UFH with high aPTT and bleeding
Actions: stop heparin; consider protamine per protocol; monitor for rebound.
Parameters: aPTT trend, visible bleeding, MAP/mentation.
Link your decisions to full scenarios in Med-Surg / Physiological Adaptation Case Studies and mixed-format practice in the NGN Case Studies hub.
NGN Tie-Ins: Action → Parameter Pairs
- Warfarin-associated bleed → actions: hold warfarin, vitamin K/reversal per protocol → parameters: visible bleeding, INR, MAP/Hgb.
- UFH overdose → actions: stop heparin, protamine per protocol → parameters: aPTT, bleeding, mentation.
- DIC pattern → actions: treat underlying cause; product support per protocol → parameters: fibrinogen, platelets, PT/aPTT, temperature, ionized Ca²⁺.
- Suspected PE → actions: oxygen, rapid workup → parameters: SpO₂/WOB, hemodynamics.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
FAQs
Is a high D-dimer diagnostic of PE/DVT?
No. It’s sensitive but not specific. Use in context with pretest probability and imaging pathways.
What INR is “therapeutic”?
It depends on the indication and your protocol (e.g., many targets are 2.0–3.0). Always verify locally.
Do DOACs change PT/INR or aPTT reliably?
Not in a way that’s helpful for routine monitoring. Follow your facility’s guidance for specialized tests and reversal.
Why is fibrinogen important in massive hemorrhage?
You can’t form stable clots without it. Consider cryoprecipitate per protocol when fibrinogen is low.