Gas embolisms, also known as air embolisms, are a critical topic for nursing students preparing for the NCLEX exam. Understanding the pathophysiology, clinical manifestations, and nursing interventions associated with gas embolisms is essential for ensuring patient safety and effective care. This comprehensive guide will delve into the essentials of gas embolisms, providing detailed explanations and practice questions to enhance your understanding. Additionally, we will include an X-ray image with a description to help you visualize and interpret this condition.
🤔 Air embolisms are rare postoperative emergencies that nurses must recognize and treat immediately.
If you want the complete, up-to-date breakdown of AI for NCLEX prep + nursing school—with independent university study metrics—use this master guide: The Ultimate Guide to AI for NCLEX Preparation and Nursing School.
What is a Gas Embolism?
A gas embolism occurs when air bubbles enter the vascular system and obstruct blood flow. This can happen due to various reasons, such as surgical procedures, trauma, or diving accidents. The presence of air in the bloodstream can lead to serious complications, including ischemia, organ dysfunction, and even death.
Pathophysiology
When air enters the bloodstream, it can travel to different parts of the body, causing blockages in blood vessels. This can lead to tissue hypoxia and damage. The severity of a gas embolism depends on the volume of air, the rate of entry, and the location of the embolism.
Clinical Manifestations
Patients with gas embolisms may present with a range of symptoms, including:
- Sudden onset of chest pain
- Dyspnea (difficulty breathing)
- Cyanosis (bluish discoloration of the skin)
- Hypotension (low blood pressure)
- Confusion or altered mental status
- Seizures
- Loss of consciousness
Diagnosis
Diagnosis of a gas embolism is primarily clinical, based on the patient's history and presenting symptoms. Imaging studies, such as X-rays, CT scans, or MRI, can help confirm the diagnosis and assess the extent of the embolism.
Treatment
Immediate treatment is crucial for patients with gas embolisms. Key interventions include:
- Placing the patient in the Trendelenburg position (head down, feet up) to prevent air from traveling to the brain.
- Administering 100% oxygen to help reduce the size of the air bubbles.
- Hyperbaric oxygen therapy (HBOT) may be used in severe cases to increase the pressure and dissolve the air bubbles.
10 NCLEX Practice Questions with Explanations
Question 1
A patient presents with sudden onset of chest pain and dyspnea after a central venous catheter insertion. What is the nurse's priority action?
A. Administer pain medication
B. Place the patient in the Trendelenburg position
C. Start an IV line
D. Call the healthcare provider
Explanation:
The correct answer is B. Placing the patient in the Trendelenburg position helps prevent air from traveling to the brain and causing further complications.
Question 2
Which of the following symptoms is most indicative of a gas embolism?
A. Fever
B. Bradycardia
C. Cyanosis
D. Edema
Explanation:
The correct answer is C. Cyanosis is a key symptom of a gas embolism, indicating reduced oxygenation of tissues.
Question 3
What is the primary purpose of administering 100% oxygen to a patient with a gas embolism?
A. To sedate the patient
B. To reduce the size of air bubbles
C. To increase blood pressure
D. To prevent infection
Explanation:
The correct answer is B. Administering 100% oxygen helps reduce the size of the air bubbles in the bloodstream.
Question 4
Which imaging study is most useful in confirming the diagnosis of a gas embolism?
A. Ultrasound
B. X-ray
C. CT scan
D. MRI
Explanation:
The correct answer is C. A CT scan is highly effective in visualizing air bubbles in the vascular system.
Question 5
During a surgical procedure, the nurse notices a sudden drop in the patient's blood pressure and oxygen saturation. What should the nurse suspect?
A. Hemorrhage
B. Gas embolism
C. Myocardial infarction
D. Pulmonary embolism
Explanation:
The correct answer is B. A sudden drop in blood pressure and oxygen saturation during surgery is indicative of a gas embolism.
Question 6
What is the role of hyperbaric oxygen therapy (HBOT) in the treatment of gas embolisms?
A. To provide pain relief
B. To dissolve air bubbles
C. To increase heart rate
D. To reduce inflammation
Explanation:
The correct answer is B. HBOT increases the pressure and helps dissolve air bubbles in the bloodstream.
Question 7
Which of the following is a common cause of gas embolisms in divers?
A. Rapid ascent
B. Dehydration
C. Hypothermia
D. Overhydration
Explanation:
The correct answer is A. Rapid ascent can cause gas bubbles to form in the bloodstream, leading to a gas embolism.
Question 8
A patient with a suspected gas embolism is placed in the Trendelenburg position. What is the rationale behind this intervention?
A. To reduce pain
B. To prevent air from traveling to the brain
C. To increase blood flow to the extremities
D. To stabilize blood pressure
Explanation:
The correct answer is B. The Trendelenburg position helps prevent air from traveling to the brain and causing further complications.
Question 9
Which of the following interventions is NOT appropriate for a patient with a gas embolism?
A. Administering 100% oxygen
B. Placing the patient in the Trendelenburg position
C. Starting an IV line
D. Encouraging deep breathing exercises
Explanation:
The correct answer is D. Deep breathing exercises are not appropriate for a patient with a gas embolism and may exacerbate the condition.
Question 10
What is the most important nursing assessment for a patient with a gas embolism?
A. Monitoring urine output
B. Assessing for signs of infection
C. Monitoring respiratory status
D. Checking blood glucose levels
Explanation:
The correct answer is C. Monitoring respiratory status is crucial for assessing the severity of the gas embolism and ensuring adequate oxygenation.
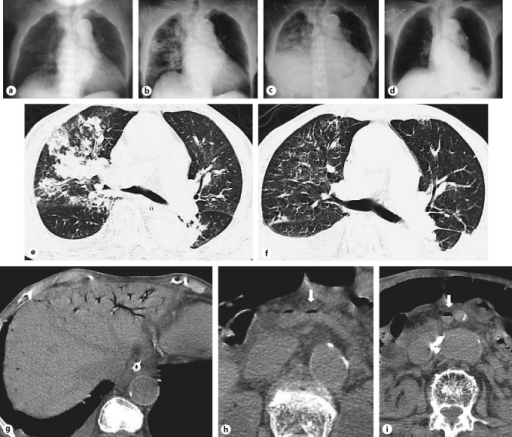
Bonus: X-Ray + Description
X-Ray Image
Chest X-ray and CT. a Chest X-ray at 11:00 am on day 1 of hospitalization, obtained 2 h before admission, shows infiltration mainly in the right upper lung field. b Chest X-ray at 1:00 p.m. on day 1 shows extensive spread of infiltration when compared with a. c Chest X-ray on day 3 shows bilateral pulmonary effusion and infiltration. d Chest X-ray on day 16 shows the disappearance of effusion and infiltration. e Plain CT of the chest on admission shows pulmonary edema located mainly on the ventral side of the right lobe of the lung along the bronchus. f Enhanced CT scan of the chest on day 13 shows bilateral pulmonary effusion and decreased pulmonary edema. g Plain CT scan of the abdomen on admission shows intrahepatic portal gas. h Plain CT scan of the abdomen on admission shows splenic vein gas (arrow). i Plain CT scan of the abdomen on admission shows superior mesenteric vein gas (arrow).
Conclusion
Understanding gas embolisms is crucial for nursing students preparing for the NCLEX exam. By familiarizing yourself with the pathophysiology, clinical manifestations, and appropriate nursing interventions, you can ensure effective patient care and improve outcomes. Use the practice questions and explanations provided in this guide to test your knowledge and enhance your readiness for the NCLEX exam. Additionally, the X-ray image and description offer valuable insights into the visualization and interpretation of gas embolisms, further solidifying your understanding of this critical condition.
By mastering the essentials of gas embolisms, you are taking a significant step towards becoming a competent and confident nurse. Good luck with your NCLEX preparation!