The Next Gen NCLEX (NGN) measures how you think at the bedside: spot the right cues, choose safe, effective actions, and pick parameters that prove your intervention worked. This pillar brings everything together—25 free case studies (with answers), item-type strategies, a conservative study plan, and links to deeper practice across med-surg, pharmacology, maternal–newborn, pediatrics, and mental health.
I’ve practiced for 20 years and taught/tutored for 10. The single biggest unlock I see? Say the priority out loud before clicking anything: “Because of A/B/C, the immediate problem is X; my two actions are Y and Z; I’ll monitor M and N in 10–30 minutes.”
Table of Contents
- What NGN Measures (and Why Case Studies Matter)
- Clinical Judgment Model (Simple 6-Step Playbook)
- NGN Item Types in Plain Language
- Scoring & Partial Credit (How Points Are Won)
- Study Plan: 4/6/8-Week NGN Blueprint
- 25 Free Case Studies by Category (with Links)
- Test-Day Strategy & Time Management
- Common Pitfalls (How to Avoid Easy Misses)
- Printable Checklists
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge—new quizzes added weekly!
What NGN Measures (and Why Case Studies Matter)
NGN cases simulate reality: evolving vitals, labs, and orders. Instead of reciting facts, you must recognize patterns and prioritize safely. That’s why practicing with case studies is high-ROI—each one forces you to run the same mental model you’ll use on the floor.
Faculty tip: Ground every decision in airway, breathing, circulation, neuro safety, and high-alert meds. If a choice doesn’t change physiology or safety, it’s probably not first.
To warm up your stem-reading skills, start with How to Read NGN Case Stems (2025): Clinical Judgment Strategy Guide.
Clinical Judgment Model (Simple 6-Step Playbook)
Use this concise loop on every screen:
- Recognize cues — pull only what matters now.
- Analyze cues — group into a likely problem pattern.
- Prioritize hypotheses — pick the most urgent issue.
- Generate solutions — list safe, effective nursing actions.
- Take action — do the highest-priority step first.
- Evaluate outcomes — choose parameters you’ll reassess in 10–30 minutes.
If you can say, “These cues → hypoxia; actions → oxygen + positioning; parameters → SpO₂ & RR,” you’re operating in NGN mode.
NGN Item Types in Plain Language
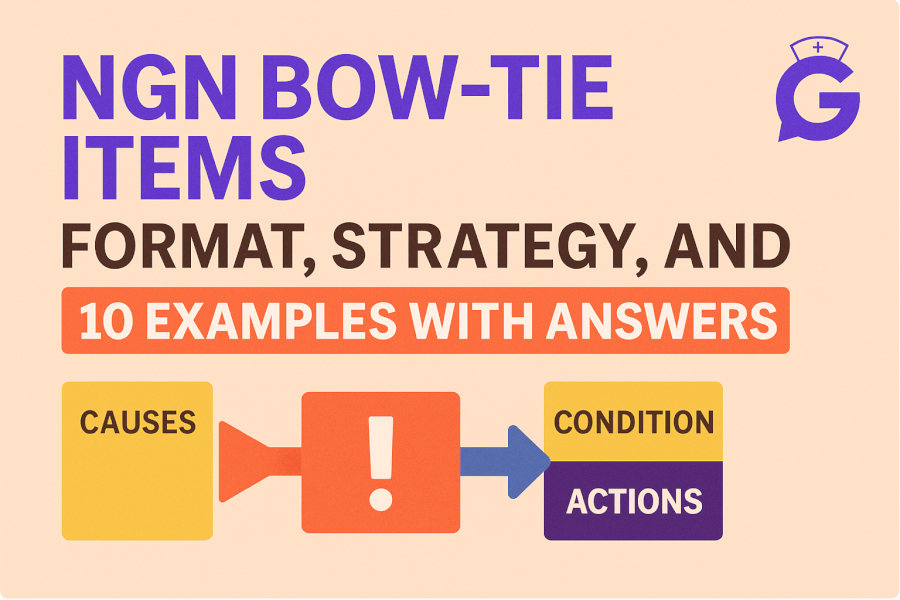
- Bow-Tie: Three boxes—Problem → Actions (x2) → Parameters (x2). Learn structure with NGN Bow-Tie Items (2025).
- Matrix/Grid: Select relevant cues/actions/rationales across rows/columns; partial credit rewards precision. Practice with NGN Matrix/Grid Items (2025).
- Trend/Highlight/Drop-down: Still the same goal—name the priority and pick the few selections that change outcomes.
Scoring & Partial Credit (How Points Are Won)
Partial credit means you can earn points even if you’re not perfect—if you pick the most relevant items. Over-selecting irrelevant boxes can reduce your net on some grids. Quality beats quantity.
Faculty tip: Your two actions should fix the physiology and prevent harm. Your two parameters should prove it worked (e.g., MAP after fluids; SpO₂/RR after oxygen).
Study Plan: 4/6/8-Week NGN Blueprint
Use conservative assumptions to avoid burnout. Pair daily micro-practice with weekly deep dives.
Daily (20–30 min):
- 1–2 NGN cases from any category.
- 1 quick lab/med refresh tied to today’s cases.
- 1 minute journaling the priority sentence for each case.
Weekly Long Block (60–120 min):
- 1 full category focus (e.g., physiological adaptation):
- 3–5 cases → rationale → redo misses.
- 10–15 min timed matrix/bow-tie drill.
- Build a mini-cheat sheet of action→parameter pairs.
Timeline options:
- 4-week sprint: 5–6 sessions/week + 2 hour weekend block.
- 6-week standard: 4–5 sessions/week + 90-minute weekend block.
- 8-week steady: 4 sessions/week + 60-minute weekend block.
When you need a pacing template, revisit How Long Should I Study for the NCLEX?.
25 Free Case Studies by Category (with Links)
Below are five core categories, each linking to 10 fully worked examples. Start with one per day; on weekends, do a timed set.
1) Stem-Reading & Foundations
- Read stems efficiently with How to Read NGN Case Stems (2025).
- Practice the bow-tie format: NGN Bow-Tie Items (2025).
- Practice matrices: NGN Matrix/Grid Items (2025).
Sample mini-cases (answers inline):
- Post-op hypoventilation → Actions: upright + oxygen; Parameters: SpO₂, RR.
- Suspected sepsis → Actions: fluids + antibiotics per order; Parameters: MAP, UOP.
2) Pharmacology (High-Alert Patterns)
Master med-driven priorities with NGN Pharmacology Case Studies (2025).
Common high-yield patterns:
- Opioids → hypoventilation/hypoxia (SpO₂/RR).
- Insulin → hypoglycemia (glucose/mentation).
- Digoxin with hypokalemia → dysrhythmia (rhythm/K⁺).
- Heparin → HIT (platelets/thrombosis).
- Lithium + dehydration/NSAIDs → early toxicity (level/neurologic status).
3) Med-Surg / Physiological Adaptation
Train for instability with NGN Med-Surg / Physiological Adaptation Case Studies (2025).
High-frequency patterns:
- Pulmonary edema → oxygen + diuretic; Parameters: SpO₂, WOB.
- GI bleed shock → large-bore IVs + fluids; Parameters: MAP, UOP.
- DKA → fluids then insulin; Parameters: K⁺, gap, glucose.
- ICP rise → position/oxygenation; Parameters: neuro checks, MAP.
4) Maternal–Newborn
Work OB/NN priorities with NGN Maternal–Newborn Case Studies (2025).
Watch for:
- Mag toxicity → stop infusion + calcium gluconate prep; Parameters: RR, DTRs.
- PPH/atony → fundal massage + uterotonics; Parameters: bleeding, MAP.
- Variable decels → reposition + O₂; Parameters: FHR variability/decels.
- Tachysystole on oxytocin → stop oxytocin + fluid bolus; Parameters: FHR, uterine tone.
5) Pediatrics & Psych
Blend safety and development with NGN Pediatrics & Psych Case Studies (2025).
Classic signals:
- Croup vs epiglottitis → humidified air vs don’t touch airway + call anesthesia.
- RSV bronchiolitis → suction + O₂; Parameters: WOB, SpO₂.
- Suicidal ideation (plan + means) → 1:1 observation + remove means; Parameters: intent, behavior.
- Alcohol withdrawal → benzo protocol; Parameters: CIWA, vitals.
Faculty tip: Build a personal “Action → Parameter” grid for each category. Your speed and accuracy will jump within a week.
Test-Day Strategy & Time Management
- Macro pace: ≈2 minutes per scored interaction. If you hit 3 minutes, make your safest clinical decision and proceed—partial credit protects you.
- Micro loop: Read stem (25–30 s) → state priority (10 s) → pick 3–5 high-yield selections (60–70 s) → sanity check (10–15 s).
- Stabilize first: Airway/oxygenation and perfusion steps beat notifications when deterioration is present.
- Don’t over-click: Extra, unrelated cues/actions silently bleed points on some matrices.
- Reset between screens: One miss doesn’t define your test. Breathe, name the next priority, move on.
Common Pitfalls (How to Avoid Easy Misses)
- Cue hoarding: If a cue doesn’t change your priority, skip it.
- Provider-first reflex: Do the safe nursing step you can implement now before calling.
- “Pretty numbers”: “Normalish” values can still be unsafe given trend and context.
- Medication tunnel vision: High-alert meds (opioids, insulin, anticoagulants, magnesium) often change the priority.
- Ignoring parameters: Always choose what you’ll reassess soon; otherwise you can’t prove success.
Printable Checklists
Universal NGN Checklist
- Identify timeline and trend words.
- Mark red-flag cues (airway, perfusion, neuro, sepsis, high-alert meds).
- State one priority hypothesis in 7–12 words.
- Choose two actions that change physiology/prevent harm.
- Choose two parameters you’ll reassess in 10–30 min.
- Document response and next step.
Action → Parameter Pairs (starter set)
- Oxygenation → SpO₂, RR/WOB
- Perfusion/fluids → MAP/BP, UOP
- Opioid sedation → RR/sedation score, SpO₂
- DKA insulin → K⁺, anion gap/glucose
- PPH uterotonics → bleeding amount, MAP/HR
- Fetal distress repositioning → FHR variability/decels, uterine tone
FAQs
How many actions and parameters should I pick?
Usually two and two unless the screen says otherwise. Pick steps that stabilize the priority and measures that change quickly.
Is “call the provider” ever first?
Yes—when there’s an immediate need you can’t address (e.g., anaphylaxis needing epinephrine per protocol, airway you can’t secure). But when you can stabilize (oxygen, positioning, fluids), do it first.
How do I study without burning out?
Short daily micro-sets + one weekly long block. Rotate categories and keep a running “Action → Parameter” sheet to compress recall time.
What if I’m slow on matrices?
State the priority aloud, then select only items that support it. If torn, pick what fixes physiology first.