Bow-tie items test whether you can pull the key problem, choose the two best nursing actions, and set the most relevant monitoring parameters to evaluate improvement. Think in three boxes: Problem → Actions → Parameters. The goal is safe, targeted decision-making you can defend at the bedside.
Faculty tip: When tutoring NCLEX candidates, I ask them to verbalize one sentence: “Because of these cues, the problem is X; my two actions are Y/Z; I’ll monitor A/B to prove it worked.”
Table of Contents
- How Bow-Tie Items Work
- A Repeatable Strategy
- 10 Practice Bow-Tie Examples (with Answers)
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge—new quizzes added weekly!
How Bow-Tie Items Work
- Left box (Problem): Identify the most likely/most urgent problem from the stem.
- Center (Actions): Choose two nursing actions that are safe, effective, and address the priority.
- Right box (Parameters): Choose two parameters to evaluate improvement or deterioration.
Faculty tip: One action should usually improve the physiology (e.g., oxygenation), the other should reduce cause or prevent harm (e.g., hold opioid, start fluids per order).
A Repeatable Strategy
- Scan for red-flags: airway/breathing, perfusion, acute neuro change, sepsis, high-alert meds.
- Name the problem in one line: “Post-op hypoventilation causing hypoxia.”
- Pick two actions: least-invasive, most effective, within nursing scope now.
- Pick two parameters: numbers you’ll watch in 10–30 minutes that prove success/failure.
- Avoid noise: skip unrelated tasks/parameters.
For category context and weightings, see:
- https://goodnurse.com/article/2/nclex-categories
- https://goodnurse.com/article/112/physiological-adaptation-definitions-key-concepts-and-mnemonics
10 Practice Bow-Tie Examples (with Answers)
1) Post-op hypoxia (opioid effect)
Stem: 64-year-old 30 minutes after morphine; shallow respirations; RR 26; SpO₂ 88% RA; drowsy.
Problem (choose 1): Hypoventilation with hypoxia.
Actions (choose 2): Elevate HOB; apply supplemental oxygen per protocol.
Parameters (choose 2): SpO₂; RR/sedation score.
Faculty tip: Fix oxygenation before calling the provider; reassess sedation after non-drug steps.
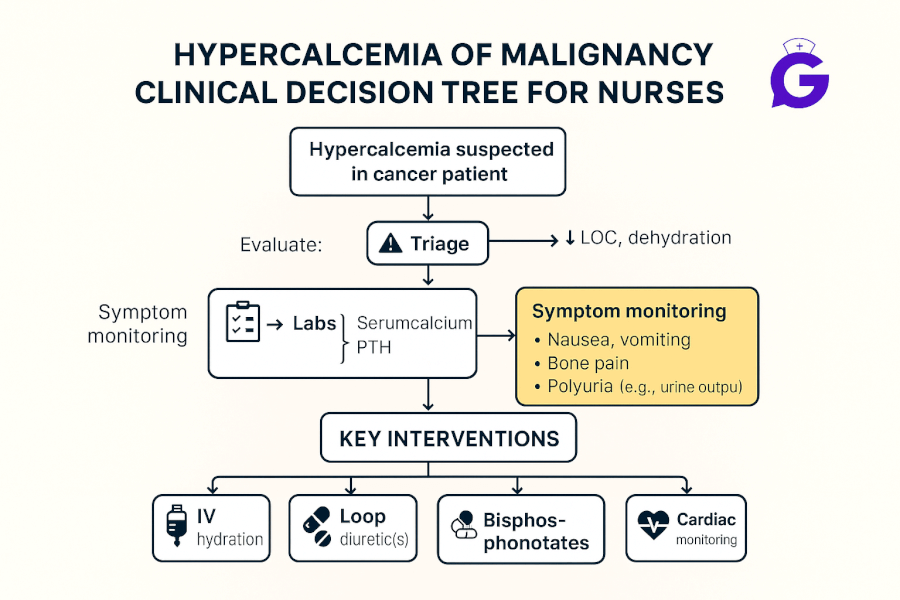
2) Sepsis concern (UTI source)
Stem: 79-year-old; temp 39.1 °C, HR 118, BP 94/56, RR 24, new confusion.
Problem: Suspected sepsis with hypoperfusion.
Actions: Begin IV fluids per order; obtain cultures/start antibiotics per order.
Parameters: MAP/BP; urine output.
Faculty tip: On NGN, fluids + antibiotics (per order) beat “call the provider” when shock is evolving.
3) Hyperkalemia on telemetry
Stem: CKD; K⁺ 6.1 mEq/L, peaked T-waves, HR 54.
Problem: Risk for dysrhythmia due to hyperkalemia.
Actions: Continuous cardiac monitoring; administer insulin with dextrose per order.
Parameters: Telemetry rhythm; serum potassium.
4) Hypoglycemia after insulin
Stem: Diaphoretic, shaky, confused; POC glucose 48 mg/dL.
Problem: Acute hypoglycemia.
Actions: Give fast-acting carbohydrate (or dextrose IV if NPO); recheck glucose in 15 minutes.
Parameters: Capillary glucose; mental status.
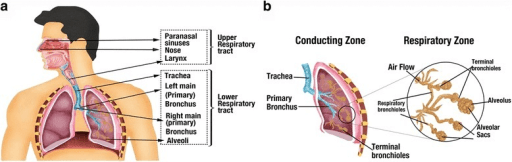
5) COPD exacerbation with CO₂ retention
Stem: Increased dyspnea, drowsy, RR 10, SpO₂ 90% on 2 L; shallow breaths.
Problem: Hypoventilation/CO₂ retention.
Actions: Elevate HOB, encourage pursed-lip breathing; titrate oxygen per protocol.
Parameters: SpO₂; RR/level of consciousness.
Faculty tip: Don’t over-oxygenate a chronic retainer—but don’t under-treat hypoxia either. Titrate and reassess.
6) DVT with suspected PE
Stem: Sudden pleuritic chest pain, tachycardia, SpO₂ 88% RA; hx DVT.
Problem: Probable pulmonary embolism.
Actions: Apply oxygen; limit ambulation/prepare for imaging and anticoagulation per orders.
Parameters: SpO₂; RR/HR.
7) Postpartum hemorrhage risk
Stem: Fundus boggy, heavy lochia, BP trending down.
Problem: Uterine atony causing hemorrhage risk.
Actions: Fundal massage; notify provider/prepare uterotonics per orders; ensure IV access.
Parameters: Amount of bleeding; BP/HR.
8) Pediatric dehydration (gastroenteritis)
Stem: Toddler lethargic, dry mucosa, cap refill >3 s, decreased UOP.
Problem: Moderate dehydration with risk for hypovolemia.
Actions: Start IV fluids per order; strict I&O with oral rehydration as tolerated.
Parameters: Urine output; capillary refill/HR.
9) Digoxin toxicity suspicion
Stem: N/V, blurred vision (yellow halos), irregular pulse; digoxin use, K⁺ 3.1.
Problem: Possible digoxin toxicity precipitated by hypokalemia.
Actions: Hold digoxin; notify provider, obtain dig level/EKG; replace potassium per order.
Parameters: Rhythm/HR; digoxin level/serum potassium.
10) Anaphylaxis after antibiotic
Stem: Wheezing, urticaria, hypotension shortly after first dose.
Problem: Acute anaphylaxis.
Actions: Stop infusion; administer epinephrine per protocol; apply high-flow O₂; prepare for fluids.
Parameters: Airway/SpO₂; BP/HR.
Faculty tip: Bow-tie scoring rewards decisive airway/perfusion steps. Don’t bury them under routine tasks.
Looking for structured weekly pacing that includes NGN work? Try:
FAQs
How many actions should I pick on bow-tie items?
Usually two. Choose the safest, most effective actions that address the priority.
Do parameters always have to be numbers?
Often numeric (SpO₂, MAP, urine output), but mental status and pain scale can be valid if they reflect the response to your action.
What’s the most common mistake?
Picking good actions that don’t match the priority. Name the problem first; the right actions follow.