I have taught this topic to dozens of cohorts. The students who score highest on NGN questions do two things well: they spot the earliest clue of toxicity and they name their next three actions in order. You are about to practice both.
Before you dive in, skim our NGN format primers so you can read stems like a pro:
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
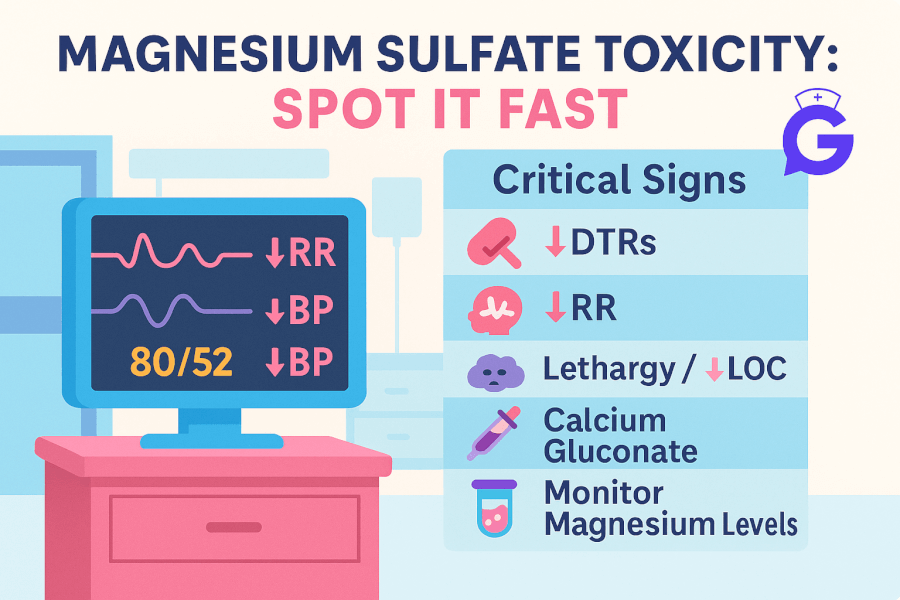
What counts as toxicity on magnesium sulfate
When a patient is on magnesium sulfate for preeclampsia or eclampsia prophylaxis, I keep three safety anchors front and center:
- Deep tendon reflexes trending down or absent
- Respiratory rate trending down toward 12 or below
- Urine output under 30 mL per hour
These are the classic bedside checks you will see in obstetric safety programs and in standard teaching references. They are reliable because they reflect magnesium’s neuromuscular and respiratory depressant effects.
I also remember the typical serum levels that are often taught alongside clinical findings. You will not titrate by level for NCLEX, but the framework helps:
- Loss of patellar reflexes often appears around 9.6 to 12 mg/dL
- Respiratory depression can appear around 12 to 18 mg/dL
- Risk of cardiac arrest rises around 24 to 30 mg/dL
These cut points show why reflexes, respirations, and urine output are your core checks.
Fun fact I always share: Magnesium relaxes smooth muscle. That helps prevent seizures in eclampsia, which is exactly why we use it. The same property can depress respirations and reflexes if levels climb too high. In eclampsia, magnesium is the anticonvulsant of choice and has better outcomes than older alternatives like diazepam or phenytoin.
The bedside safety loop I use every time
I keep a simple loop in my notes: Assess → Trend → Decide → Act → Reassess.
Within that loop, here is the checklist I teach new grads to use during magnesium therapy:
- Respirations every 1 to 2 hours, more often if drowsy
- Patellar reflexes at routine intervals and if sedation deepens
- Urine output hourly if Foley is present, or frequent checks if not
- Level of consciousness and symptom screen for new lethargy, slurred speech, visual changes
- Calcium gluconate available at the bedside and actively verified on every handoff
The exact stop and rescue sequence
If I suspect toxicity, my internal monologue goes like this:
- Stop the magnesium infusion immediately
- Call for help and notify the provider while I continue airway, breathing, and circulation
- Prepare and administer calcium gluconate per standing orders or protocol
- Support airway and breathing and be ready to escalate respiratory support
- Reassess frequently because symptoms can recur while serum magnesium remains elevated
About the antidote: Many quality collaboratives reference calcium gluconate 1 gram IV over about 3 minutes, with repeat dosing if needed. Exact dosing follows unit protocol and provider orders. For NCLEX, memorize that calcium gluconate is the antidote, and the first move is to stop the infusion and escalate.
NGN Bow-Tie Practice: Spot, Act, and Prevent
Below are three quick bow-tie drills. If you need a refresher on structure, open our bow-tie walkthrough.
Bow-Tie 1: Early clue, fast action
Stem: Primigravida at 35 weeks on magnesium sulfate for severe preeclampsia. Findings: RR 14 and trending down from 16, patellar reflexes 1 plus from prior 2 plus, urine output 28 mL per hour over the last hour. The patient says she feels heavier and very sleepy.
Left side: Risks and cues to recognize
- Respirations trending down toward 12
- DTRs dulled from baseline
- Urine output under 30 mL per hour
Right side: Actions and monitoring
- Stop magnesium infusion and call the provider
- Keep calcium gluconate at the bedside and prepare per protocol
- Reassess respirations, airway, oxygen saturation, and level of consciousness every few minutes
- Document changes and notify the charge nurse
Center: Expected outcomes
- Respirations stabilize above 12 per minute
- Reflexes return toward baseline
- Urine output improves with close fluid balance monitoring
Bow-Tie 2: The antidote is ready
Stem: Patient on postpartum magnesium infusion is now difficult to arouse. RR 10. No patellar reflexes. Blood pressure is stable. SpO₂ 93 percent on room air. The provider is en route.
Left: Key cues
- Respirations below 12
- Absent DTRs
- Increasing sedation
Right: Actions
- Stop the magnesium infusion
- Prepare and administer calcium gluconate per protocol
- Elevate the head of bed, apply oxygen, and monitor closely
- Have airway equipment available and alert rapid response as indicated
Center: Expected outcomes
- Improved respiratory rate
- Return of reflexes over time as magnesium level falls
- Prevention of respiratory arrest
Bow-Tie 3: Do I stop magnesium during a seizure
Stem: A patient with eclampsia begins tonic clonic activity during a room transfer. She is on a therapeutic magnesium infusion. The team arrives.
Left: Key cues
- Active seizure in a preeclamptic patient
- On magnesium, but seizure is breaking through
Right: Actions
- Protect the airway and the patient from injury, position laterally, call for help
- Follow seizure management protocol, including a magnesium bolus if ordered
- Prepare to suction and support breathing, check glucose per protocol
- Postictal assessment and fetal status if applicable
Center: Expected outcomes
- Seizure control
- Airway protected and oxygenation maintained
- Ongoing evaluation to prevent recurrence
Quick tables you can memorize
Table 1. Is my patient slipping into toxicity
| Clue | Why I care | My next moves |
|---|---|---|
| DTRs from 2 plus to 1 plus or absent | Neuromuscular junction is depressed | Stop infusion, reassess, prepare antidote, call the provider |
| Respirations falling toward 12 or under 12 | Respiratory depression risk | Airway, oxygen, stop infusion, antidote per protocol |
| Urine output under 30 mL per hour | Magnesium excretion may be impaired | Call the provider, consider holding dose, monitor intake and output and renal function |
| New lethargy or slurred speech | Central nervous system depression | Frequent reassessment and escalation as indicated |
Table 2. What must be at the bedside
- Primary IV with the correct line set
- Magnesium infusion pump programmed and verified
- Calcium gluconate immediately available
- Airway supplies accessible and oxygen source checked
- Reflex hammer and a clear documentation flowsheet
Postpartum twist students miss on exams
Many stems move the patient to postpartum and test whether you continue magnesium and for how long. Practice environments vary on exact timing, which is why you first anchor to local orders. Teaching summaries and clinical guidance commonly maintain continuation through the immediate postpartum window, with duration tailored to severity and the provider plan. Your exam priority is to keep safety monitoring in place, maintain antidote readiness, and avoid premature discontinuation.
If you want more depth on postpartum handoffs, read our upcoming spoke on Postpartum on Mag and review prioritization skills here:
FAQ I get from students
Do I check a serum magnesium level or rely on clinical findings
For exams, prioritize clinical signs that track with therapeutic effect and toxicity. Reflexes, respirations, and urine output are frontline. Some settings check levels on an interval, but NCLEX commonly tests your bedside recognition and immediate actions.
Is magnesium still first line in eclampsia over other anticonvulsants
Yes. Reviews and summaries consistently support magnesium sulfate as the anticonvulsant of choice for preventing recurrent seizures in eclampsia.
What is the exact calcium gluconate dose. Do I have to memorize it
Quality collaboratives frequently reference 1 gram IV over a few minutes, with repeat dosing if needed. Your unit protocol will control the specifics. For NCLEX, know that calcium gluconate is the antidote and that you should stop the infusion and escalate immediately.
Do I ever keep magnesium going during concerns for toxicity
If you have credible signs of toxicity, you stop the infusion and treat. If the issue is a within range side effect such as flushing or mild nausea, you continue monitoring and reassess. Know the difference and escalate concerns quickly.
Bring it all together with cross practice
- Refresh pattern recognition with our Electrolytes Cheat Sheet and the full Electrolyte Pillar.
- If respirations dip, practice the ABG angle so you can explain why a respiratory rate of 10 is dangerous: ABG Interpretation: 15 Cases.
- Level up your NGN format confidence with our Bow-Tie and Matrix or Grid guide.
- Reinforce clinical judgment with our Med-Surg case bank and Pharmacology case bank.
Key takeaways
- Earliest reliable clues are falling reflexes, falling respirations, and low urine output.
- Stop the infusion first, then escalate and prepare calcium gluconate while protecting airway and breathing.
- Antidote readiness is not optional. Keep it at the bedside and verify during every handoff.
- Seizures can break through therapy. Magnesium remains first line, and seizure management follows protocol with airway protection.
- Postpartum monitoring and continuation are common. Do not abandon surveillance early.
If you want the complete, up-to-date breakdown of AI for NCLEX prep + nursing school—with independent university study metrics—use this master guide: The Ultimate Guide to AI for NCLEX Preparation and Nursing School.
Further Reading on GoodNurse
- Electrolytes Cheat Sheet: Patterns and Nurse Actions
- Electrolyte Pillar: Ultimate Guide
- How to Read NGN Case Stems
- NGN Bow-Tie Items Explained
- Med-Surg Case Studies
- Pharmacology Case Studies
- ABG Interpretation: 15 Practice Cases
References
- Agency for Healthcare Research and Quality. Safe Medication Administration: Magnesium Sulfate. Standing orders and what to do if toxicity is suspected. https://www.ahrq.gov/patient-safety/settings/labor-delivery/perinatal-care/modules/strategies/medication/tool-safe-mgso4.html
- AHRQ. Safety Program for Perinatal Care: Safe Medication Administration Facilitator Guide. Readiness elements and escalation concepts. https://www.ahrq.gov/patient-safety/settings/labor-delivery/perinatal-care/modules/strategies/medication/safe-medication-fac-guide.html
- NCBI Bookshelf, StatPearls. Magnesium Sulfate and Magnesium Toxicity. Clinical monitoring with reflexes, respirations, and urine output. https://www.ncbi.nlm.nih.gov/books/NBK554553/ and https://www.ncbi.nlm.nih.gov/books/NBK554593/
- Florida Perinatal Quality Collaborative, USF Health. Magnesium Sulfate quality document with toxicity manifestations and antidote dosing examples. https://health.usf.edu/-/media/Files/Public-Health/Chiles-Center/FPQC/Magnesium_Sulfate.ashx
- American College of Obstetricians and Gynecologists. Gestational Hypertension and Preeclampsia. Practice guidance on indications and management context. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2020/06/gestational-hypertension-and-preeclampsia
- Cochrane Review hosted on NIH PMC. Magnesium sulfate is the anticonvulsant of choice for eclampsia. https://pmc.ncbi.nlm.nih.gov/articles/PMC7061250/