Maternal–newborn cases test calm, priority-driven nursing: protect airway and perfusion, anticipate hemorrhage or seizure, and safeguard the newborn’s transition. After 20 years at the bedside and 10 as a professor/tutor, I tell students: name the one priority, act on it, and pick parameters that prove your action worked within 10–30 minutes. If you’re new to stem reading, start with How to Read NGN Case Stems (2025): Clinical Judgment Strategy Guide, then layer format skills with NGN Bow-Tie Items (2025) and NGN Matrix/Grid Items (2025).
Table of Contents
- How to Use These Case Studies
- Case 1: Preeclampsia on Magnesium—Toxicity Risk
- Case 2: Postpartum Hemorrhage (Uterine Atony)
- Case 3: Shoulder Dystocia—Intrapartum Emergency
- Case 4: Fetal Distress—Variable Decelerations
- Case 5: Chorioamnionitis—Maternal Fever in Labor
- Case 6: Uterine Tachysystole on Oxytocin
- Case 7: Postpartum Infection—Endometritis
- Case 8: Newborn Hypoglycemia—Infant of Diabetic Mother
- Case 9: Neonatal Respiratory Distress—TTN vs. RDS
- Case 10: Hyperbilirubinemia—Breastfeeding Jaundice
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge—new quizzes added weekly!
How to Use These Case Studies
- Read once for timeline (intrapartum, immediate PP, 24–72h PP) and trend words (“worsening,” “after medication”).
- State the priority aloud in one sentence; pick two actions and two monitoring parameters you can reassess soon.
- If you need a fast blueprint refresher, skim NCLEX Categories & Subcategories (Weights, Examples, Practice); for instability patterns, see Physiological Adaptation: Key Concepts & Mnemonics.
Case 1: Preeclampsia on Magnesium—Toxicity Risk
Stem (condensed): Laboring client on magnesium sulfate. Reports muscle weakness; RR 10; DTRs 1+; urine output 20 mL/hr; drowsy.
Priority problem: Magnesium toxicity with risk of respiratory depression.
Two best actions:
- Stop magnesium infusion; notify provider; prepare calcium gluconate per protocol.
- Support airway/oxygenation; reassess DTRs and RR frequently.
Two parameters: RR/SpO₂; DTRs/mental status; urine output.
Rationale: Halt/antagonize toxicity and protect ventilation.
Faculty tip: When I teach magnesium checks, I use “DTRs, Drowsy, Diuresis.” Abnormal in two out of three? Slow down or stop the drip.
Case 2: Postpartum Hemorrhage (Uterine Atony)
Stem: Vaginal delivery 45 minutes ago; boggy fundus, heavy lochia with clots, BP trending down, HR 120; perineal pad saturated in 15 minutes.
Priority problem: Uterine atony causing acute hemorrhage.
Two best actions:
- Fundal massage until firm; assess for retained fragments; ensure empty bladder.
- Activate PPH protocol: large-bore IV access, uterotonics per order (oxytocin first-line; then methylergonovine if no HTN; carboprost if no asthma), type & cross.
Two parameters: Amount of bleeding; fundal tone/height; BP/HR (MAP).
Rationale: Mechanical tone + medications reduce bleeding; volume support prevents shock.
- For med-surg instability patterns that often intersect with OB emergencies, practice with NGN Med-Surg / Physiological Adaptation Case Studies (2025): 10 Examples with Answers and Rationale.
Case 3: Shoulder Dystocia—Intrapartum Emergency
Stem: “Turtle sign” during delivery; head delivers then retracts; no progress with gentle traction.
Priority problem: Obstructed shoulder risking fetal hypoxia and brachial plexus injury.
Two best actions:
- Call for help; instruct mother stop pushing; perform McRoberts (hyperflex maternal hips) with suprapubic pressure.
- Prepare for additional maneuvers per provider (Wood’s corkscrew, delivery of posterior arm).
Two parameters: Fetal heart rate; time from head to body delivery; maternal status (perineal trauma/bleeding).
Rationale: McRoberts and suprapubic pressure widen pelvic outlet; minimize traction injury.
Case 4: Fetal Distress—Variable Decelerations
Stem: Intermittent variable decelerations with minimal variability; suspected cord compression.
Priority problem: Compromised fetal oxygenation due to cord compression.
Two best actions:
- Reposition (side-to-side, knee-chest if severe); oxygen by mask if persistent; stop oxytocin if infusing.
- IV fluid bolus per order; consider amnioinfusion if ordered.
Two parameters: FHR pattern variability/decels; uterine activity; maternal vitals/response.
Rationale: Relieve cord pressure and improve placental perfusion.
Case 5: Chorioamnionitis—Maternal Fever in Labor
Stem: Maternal temp 38.5°C, maternal/fetal tachycardia, uterine tenderness, foul-smelling fluid; prolonged ROM.
Priority problem: Intra-amniotic infection with risk to parent and fetus.
Two best actions:
- Administer broad-spectrum antibiotics per order; antipyretics and IV fluids.
- Continuous fetal monitoring; prepare for delivery if indicated by maternal/fetal status.
Two parameters: Maternal temp/HR and WBC; FHR baseline/variability; amniotic fluid findings.
Rationale: Treat infection, reduce fever, and evaluate fetal tolerance of labor.
Case 6: Uterine Tachysystole on Oxytocin
Stem: On oxytocin; contractions every <2 minutes, lasting >90 seconds, resting tone elevated; FHR late decelerations.
Priority problem: Uteroplacental insufficiency from excessive uterine activity.
Two best actions:
- Stop oxytocin; reposition left lateral; IV bolus per order; oxygen by mask.
- If unresolved, prepare for tocolytic per order and provider evaluation.
Two parameters: FHR pattern; contraction frequency/duration and resting tone; maternal BP.
Rationale: Reduce uterine activity to restore fetal oxygenation.
Case 7: Postpartum Infection—Endometritis
Stem: Postpartum day 2; foul lochia, uterine tenderness, fever, malaise; C-section 2 days ago.
Priority problem: Endometritis (uterine infection) risk.
Two best actions:
- Obtain cultures as ordered; start broad-spectrum IV antibiotics per protocol.
- Encourage ambulation and hydration; antipyretics per order; monitor incision if C-section.
Two parameters: Temp trend; uterine tenderness/fundal height; lochia character; WBC.
Rationale: Treat infection and prevent complications (abscess, sepsis).
Case 8: Newborn Hypoglycemia—Infant of Diabetic Mother
Stem: Term infant of diabetic mother; jittery, poor feeding, weak cry; first glucose 32 mg/dL at 45 minutes of life.
Priority problem: Neonatal hypoglycemia risking neurologic injury.
Two best actions:
- Immediate feeding (breast or formula) if able; if symptomatic or unable to feed, IV dextrose per order.
- Skin-to-skin for thermoregulation and glucose stability; frequent checks.
Two parameters: Blood glucose trend; level of alertness/tone; feeding effectiveness.
Rationale: Provide fast glucose and minimize energy expenditure/heat loss.
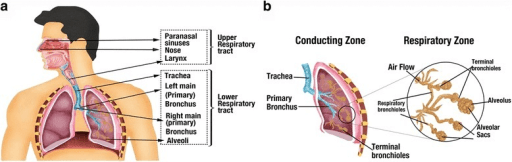
Case 9: Neonatal Respiratory Distress—TTN vs. RDS
Stem: Late preterm, cesarean without labor; tachypnea (RR 75), mild retractions, grunting; pulse ox 90–92% on room air.
Priority problem: Impaired gas exchange—likely TTN (transient tachypnea) vs early RDS.
Two best actions:
- Provide warmth and supplemental oxygen to maintain target sats; minimal stimulation.
- Notify provider; prepare for CPAP if ordered; monitor for fatigue/apnea.
Two parameters: Respiratory rate/retractions; SpO₂; ABG/cap gas if ordered.
Rationale: Support oxygenation while fluid clears (TTN) or escalate if RDS emerges.
Case 10: Hyperbilirubinemia—Breastfeeding Jaundice
Stem: Term infant day 3; poor latch, <6 wet diapers/day, weight loss 8–9%; visible jaundice to chest; TSB borderline high for age.
Priority problem: Suboptimal intake leading to early hyperbilirubinemia.
Two best actions:
- Lactation support now; increase feeding frequency; consider supplementation per pediatric guidance.
- Phototherapy if thresholds met; parent education on outputs and jaundice progression.
Two parameters: Bilirubin trend; weight change/diaper counts; feeding quality.
Rationale: Improve intake and bilirubin elimination; treat promptly to prevent kernicterus.
Faculty tip: When torn between two plausible actions, choose the one that changes physiology first (airway, perfusion, neuro) and that you can measure within 10–30 minutes. For pharmacology-heavy OB scenarios (magnesium, oxytocin, antihypertensives), a quick refresher is here: NGN Pharmacology Case Studies (2025).
FAQs
How many actions and parameters should I select on NGN OB items?
Usually two and two unless specified. Pick steps that address the immediate risk (airway, perfusion, seizure/hemorrhage) and parameters that show early response (SpO₂, MAP, uterine tone, FHR).
Is “call the provider” ever the first action?
Yes—after you’ve taken the safe nursing step you can implement immediately (stop oxytocin, reposition, oxygen, fundal massage, airway support).
How do I balance fetal and maternal priorities?
Stabilize the parent to stabilize the fetus: restore oxygenation and perfusion first, then escalate.
How can I practice efficiently without burning out?
Use daily micro-sets (10–20 minutes) and one longer block weekly. For pacing that includes NGN, see How Long Should I Study for the NCLEX?.