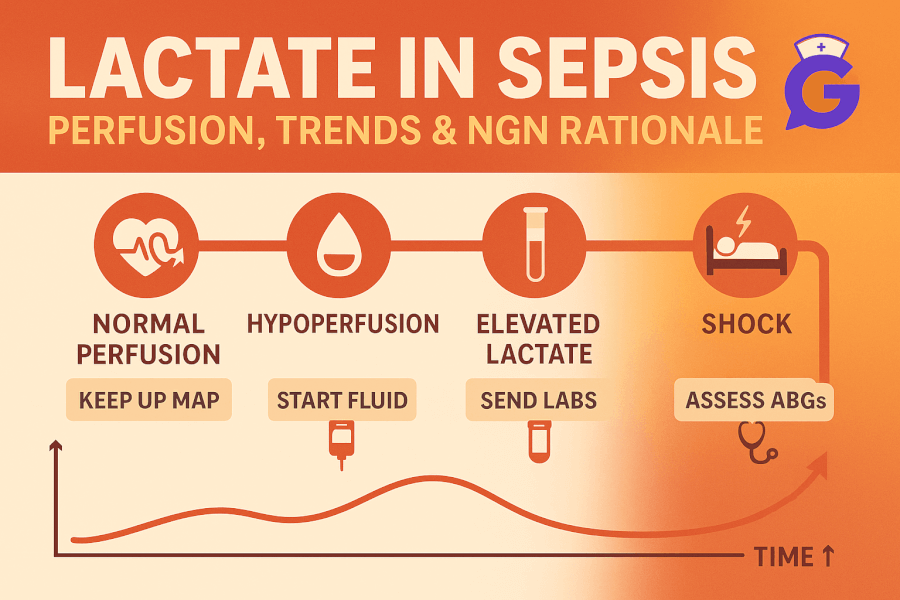
Lactate is a perfusion clue, not a verdict. High values can reflect hypoperfusion and oxygen debt—exactly what you’re trying to reverse early in suspected sepsis. This guide shows what lactate actually means, how to avoid false positives, and how to choose actions that change physiology with parameters that prove it worked—an NGN habit that also plays out at the bedside.
If you need acid–base context, pair this with ABG Interpretation Made Simple (2025). For related labs and organ-function signals, keep Renal Function & UA Interpretation (2025) and Coagulation Studies (2025) open.
Table of Contents
- What Lactate Tells You (and Doesn’t)
- Quick Reference: Levels, Trends, Triggers
- When and How to Draw Lactate
- Interpreting Elevated Lactate (Patterns & Pitfalls)
- First Hour Priorities (Nursing View)
- NGN Tie-Ins: Action → Parameter Pairs
- Sample SBAR & Charting Tips
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
What Lactate Tells You (and Doesn’t)
Plain language: Lactate rises when tissues can’t meet energy demands—often due to poor perfusion and oxygen delivery. It can also rise from stress hormones and accelerated metabolism (e.g., seizures, β-agonists).
Use lactate to:
- Support the story of shock/hypoperfusion.
- Track improvement after oxygenation, fluids, vasoactive support, and source control per team plan.
- Flag clients at higher risk who need closer monitoring—even if vitals look “better” for a moment.
Professor’s note: Don’t chase a single number. Your early wins come from matching actions (oxygenation, perfusion) to parameters that move soon (SpO₂, MAP, urine output)—then letting lactate confirm the trend.
Quick Reference: Levels, Trends, Triggers
| Item | Nursing Takeaway |
|---|---|
| “Normal-ish” | Values vary by lab. A “normal” initial lactate doesn’t rule out sepsis if the story fits. Trend + assessment > one draw. |
| “Elevated” | Higher lactate often correlates with **worse perfusion**; persistent elevation after interventions is a concern—escalate. |
| Trend/“clearance” | Look for **downward movement** after you optimize oxygenation/perfusion and start therapy. No movement? Reassess causes. |
| Common non-sepsis causes | Seizures, strenuous activity, β-agonists, severe asthma, hepatic dysfunction, shock from noninfectious causes, **tourniquet/time-to-lab issues**. |
Always interpret with **symptoms, vitals, organ function, urine output, ABG**, and suspected source.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
When and How to Draw Lactate
When
- At initial suspicion of sepsis or shock picture (altered mentation, hypotension, tachypnea, fever/chills, suspected infection).
- Repeat after initial interventions to assess trajectory—time interval per local protocol.
How (collection tips)
- Arterial or venous? Venous samples are commonly acceptable for trend; confirm your facility’s policy.
- Processing: Minimize tourniquet time; get the sample to the lab quickly; avoid prolonged storage or delays.
- Document: Exact time of draw, any oxygen/fluids/vasoactives initiated, and changes in SpO₂/MAP/UOP around the draw.
Interpreting Elevated Lactate (Patterns & Pitfalls)
Pattern 1: Hypoperfusion picture
- Story: cold clammy skin, altered mentation, low MAP, oliguria; ABG may show metabolic acidosis.
- Priority: oxygenation and perfusion.
- Next steps: Position, oxygen to target, IV access, fluids per order, rapid team evaluation, prepare for vasoactives as directed.
Pattern 2: Mixed picture (sepsis + comorbidities)
- Story: infection signs plus COPD/asthma or hepatic dysfunction.
- Priority: oxygenation and work of breathing; watch β-agonist–related lactate bump vs true under-resuscitation.
- Next steps: Reassess trend, not just absolute value; document WOB, SpO₂, RR, and response to therapies.
Pattern 3: “False-high” risk
- Story: recent seizure, strenuous activity, prolonged tourniquet, delayed processing.
- Priority: confirm with repeat under cleaner conditions; don’t over-treat the lab—treat the client and story.
Pitfalls to avoid
- Anchoring on a first “normal.” Clients can deteriorate—keep trending with assessment.
- Treating the number alone. Pair lactate with MAP, UOP, mentation, skin, and ABG.
- Missing the source. Ongoing hypoperfusion plus rising lactate may point to inadequate source control or insufficient perfusion.
First Hour Priorities (Nursing View)
Your job is to optimize oxygen delivery and support perfusion while diagnostics and orders are moving.
- Airway/Breathing: Position upright, oxygen to target SpO₂. If WOB high, escalate monitoring and support per team plan.
- Circulation: Two large-bore IVs, fluids per order; monitor for response (MAP, UOP, mentation).
- Labs/Cultures: Obtain as directed by policy; don’t delay time-sensitive therapy that’s been ordered.
- Reassess early: Within minutes to hours—SpO₂, RR/WOB, MAP, UOP, mental status—and document response.
- Communicate changes promptly with trend language and action → parameter framing (see SBAR below).
Professor’s note: The “right” answer is usually the pair that moves physiology soonest—oxygenation + perfusion. Then pick parameters that will reflect that change within minutes to an hour.
NGN Tie-Ins: Action → Parameter Pairs
- Suspected sepsis with hypotension → actions: oxygen to target; fluids per order → parameters: SpO₂, MAP, UOP, mentation.
- Rising lactate despite oxygen and fluids → actions: escalate evaluation and support per team plan → parameters: MAP, UOP, lactate trend, ABG.
- High WOB with borderline oxygenation → actions: position, oxygen, treat underlying respiratory issue → parameters: SpO₂, RR/WOB, ABG.
- Possible sampling/processing error → actions: redraw, minimize tourniquet time → parameters: repeat lactate, chart exact timing and conditions.
Link your reasoning with case practice in NGN Med-Surg Physiological Adaptation Case Studies (2025) and format primers in the NGN Case Studies hub.
Sample SBAR & Charting Tips
SBAR — Elevated Lactate with Hypotension
- Situation: “Mr. J has MAP 58 with cool clammy skin; lactate elevated.”
- Background: “Fever 38.9°C, suspected pneumonia; IV access established; fluids started per order.”
- Assessment: “Concern for hypoperfusion; UOP low; mentation fluctuates; SpO₂ 91% RA.”
- Recommendation: “Request evaluation for further resuscitation and support; trending MAP, UOP, ABG planned.”
Chart the story, not just the number
- Time-stamp interventions near the draw (oxygen, fluids).
- Record MAP, UOP, SpO₂, mentation before and after interventions.
- Note collection factors (tourniquet time, delay to lab) if present.
FAQs
Does a normal first lactate rule out sepsis?
No. It’s one data point. Reassess based on the story and trend with vitals, UOP, mentation, and ABG.
Is venous lactate acceptable?
Many facilities accept venous for screening and trend; confirm your policy.
My client is on β-agonists and lactate is high. Is that sepsis?
Not necessarily. β-agonists and seizures can raise lactate. Pair with perfusion signs (MAP/UOP/mentation) and infection likelihood.
How fast should lactate fall?
Look for movement in the right direction after actions that improve perfusion and oxygenation. If it doesn’t move, reassess source and support.
What should I trend alongside lactate?
MAP, UOP, SpO₂, mentation, ABG (acid–base and ventilation), plus temperature and WBC in context.