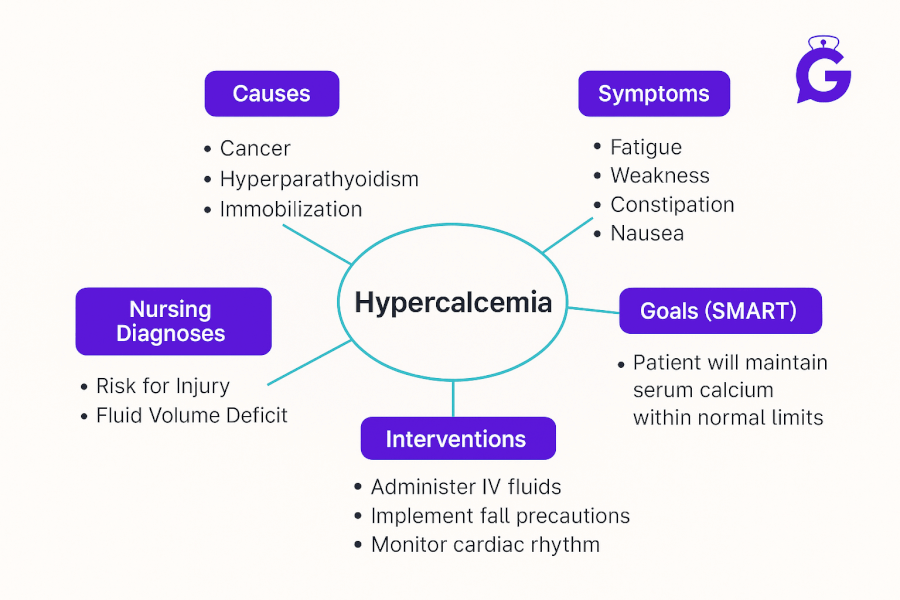
In my years as a clinical instructor, I’ve watched students freeze when a patient presents with severe hypercalcemia—weakness, constipation, confusion, even dysrhythmias. Building a care plan here isn’t busywork; it’s the blueprint that prevents falls, kidney stones, and cardiac events. In this guide, I’ll walk you through an NGN-ready Hypercalcemia Nursing Care Plan: quick pathophysiology, prioritized nursing diagnoses, SMART outcomes, and specific nursing interventions with rationales. By the end, you’ll know what to assess first, which actions change outcomes fastest, and how to teach patients and families with confidence.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
Table of Contents
- Pathophysiology of Hypercalcemia
- Nursing Care Plans (Diagnoses, Outcomes, Interventions & Rationales)
- FAQs
- Further Reading
- References
Pathophysiology of Hypercalcemia
Hypercalcemia is commonly defined as serum calcium >10.5 mg/dL, according to the Merck Manual. Leading causes are primary hyperparathyroidism and malignancy (PTHrP secretion, osteolytic metastases). Calcium excess decreases neuronal membrane excitability and GI smooth-muscle activity, impairs renal concentrating ability (polyuria → dehydration), and shortens the QT interval—raising dysrhythmia risk. Management aligns to severity and etiology: isotonic IV fluids for volume repletion, avoidance of precipitating meds (e.g., thiazides), and agents such as calcitonin or bisphosphonates/denosumab for malignancy-related disease; definitive therapy targets the cause (e.g., parathyroidectomy in primary hyperparathyroidism).
If you want the complete, up-to-date breakdown of AI for NCLEX prep + nursing school—with independent university study metrics—use this master guide: The Ultimate Guide to AI for NCLEX Preparation and Nursing School.
Assessment highlights
- Fatigue, muscle weakness, diminished DTRs, anorexia, constipation, abdominal/flank pain (stones), confusion.
- ECG: shortened QT; labs: elevated Ca²⁺, possible elevated PTH (if primary hyperparathyroidism).
- Contributors: thiazide diuretics, vitamin D or calcium supplements, prolonged immobility, malignancy.
Study support on GoodNurse: Build clinical reasoning with ABG Interpretation: 15 Practice Cases, apply NGN thinking with NGN Med-Surg Physiological Adaptation Case Studies, and explore study tools in Best AI Apps for Nursing Students (2025).
Nursing Care Plans for Hypercalcemia
Below are high-yield nursing diagnoses with SMART outcomes, interventions, and rationales for a patient with hypercalcemia. Use them to build your individualized plan of care.
Nursing Diagnosis: Acute Confusion
| Category | Details |
|---|---|
| Related to | Altered cerebral function secondary to elevated serum calcium and dehydration |
| As evidenced by | Disorientation, impaired attention, forgetfulness, safety-risk behaviors; family report of acute change |
| Desired Outcomes | Within 24–48 hrs, patient remains oriented ×4 and free from injury; CAM negative; caregiver verbalizes home safety plan. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Institute fall precautions, frequent reorientation, and close observation (consider sitter). | Cognitive changes and weakness increase injury risk; structured safety reduces harm. |
| Encourage PO fluids as ordered; initiate isotonic IV fluids if moderate–severe. | Hydration improves renal calcium excretion and reduces delirium from dehydration. |
| Cluster care, reduce stimuli, and support sleep–wake cycles. | Minimizes delirium triggers and supports reorientation. |
| Review meds/supplements (thiazides, vitamin D, calcium, antacids) and collaborate on adjustments. | Several agents exacerbate hypercalcemia; deprescribing facilitates correction. |
Nursing Diagnosis: Risk for Renal Calculi
| Category | Details |
|---|---|
| Related to | Hypercalciuria, dehydration, immobility, malignancy-related bone resorption |
| As evidenced by | (Risk factors) Elevated serum/urine calcium, low urine specific gravity, history of stones, flank discomfort |
| Desired Outcomes | Urine output ≥0.5–1 mL/kg/hr; no hematuria/flank pain; patient demonstrates stone-prevention strategies at discharge. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Start isotonic IV fluids per order; maintain strict I&O; obtain daily weights. | Volume repletion increases calcium excretion and lowers stone formation. |
| Strain urine if stones suspected; monitor for hematuria and flank pain; escalate promptly. | Early detection guides therapy and prevents obstruction/AKI. |
| Encourage mobilization and ROM exercises. | Immobility promotes bone resorption and urinary calcium loss. |
| Teach hydration goals and balanced diet (avoid unnecessary calcium/vitamin D supplements; tailor oxalate guidance if indicated). | Hydration and balanced intake reduce stone risk more effectively than severe restriction. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Nursing Diagnosis: Constipation
| Category | Details |
|---|---|
| Related to | Decreased GI smooth-muscle excitability secondary to hypercalcemia; reduced activity; inadequate fluid/fiber |
| As evidenced by | Infrequent stools, hard/dry stool, straining, abdominal discomfort, hypoactive bowel sounds |
| Desired Outcomes | Soft, formed BM q1–2 days without straining; decreased abdominal discomfort within 48–72 hrs. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Promote fluids per plan; offer warm fluids and scheduled toileting after meals. | Hydration and the gastrocolic reflex support stool softening and transit. |
| Encourage fiber-rich foods as tolerated; collaborate on stool softeners/osmotic laxatives. | Improves stool consistency and reduces straining. |
| Increase ambulation within safety limits. | Activity stimulates bowel motility and counters hypercalcemia-related slowing. |
Nursing Diagnosis: Deficient Knowledge
| Category | Details |
|---|---|
| Related to | Unfamiliarity with condition, medications (calcitonin, bisphosphonates/denosumab), hydration and mobility needs |
| As evidenced by | Questions about diet/supplements and safety; inconsistent adherence to fluid/mobility plan |
| Desired Outcomes | Patient/family accurately teach back hydration goals, medication plan, activity guidance, and return precautions before discharge. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach hydration targets and urine monitoring; avoid unnecessary calcium/vitamin D supplementation unless prescribed. | Supports maintenance therapy and stone prevention; reduces recurrence risk. |
| Review medication purpose/timing and adverse effects (e.g., transient flushing with calcitonin; rare jaw osteonecrosis with long-term bisphosphonates). | Improves adherence and early reporting of serious effects. |
| Provide written return precautions: worsening confusion, palpitations, severe constipation, decreased urine, flank pain. | Early escalation prevents complications (arrhythmias, obstruction, AKI). |
Frequently Asked Questions (FAQ)
What is the priority nursing intervention for hypercalcemia?
The absolute priority is patient safety and initiating isotonic IV fluids (e.g., 0.9% Normal Saline) as prescribed. Hypercalcemia causes muscle weakness and confusion, creating a high fall risk. Hydration promotes renal excretion of calcium and helps correct the underlying problem.
Why is a patient with hypercalcemia at risk for dysrhythmias?
Calcium is key for cardiac muscle contraction. Hypercalcemia shortens the QT interval on ECG, increasing risk for dangerous ventricular dysrhythmias—hence continuous monitoring for severe cases.
What ECG changes are seen with hypercalcemia?
A shortened QT interval is classic; severe cases may progress to ventricular dysrhythmias. Always correlate with symptoms, labs, and provider orders for monitoring.
What fluids are given for hypercalcemia?
Isotonic IV fluids (typically 0.9% Normal Saline) are first-line to correct dehydration and increase urinary calcium excretion. Rate and total volume depend on age, comorbidities, and provider orders.
Which medication lowers calcium the fastest?
Calcitonin works quickly (hours) but with a short-lived effect; IV bisphosphonates (e.g., zoledronic acid) or denosumab provide a more sustained reduction in malignancy-related hypercalcemia—always per provider order and institutional protocol.
Further Reading
- ABG Interpretation: 15 Practice Cases (with Rationale)
- NGN Med-Surg Case Studies: Physiological Adaptation
- NGN Pharmacology Case Studies: 10 Examples with Answers
- Pediatric Dosage Calculations for NCLEX (20 Scenarios)
- Best AI Apps for Nursing Students (2025)