Diabetes is a chronic condition that affects millions of people worldwide. As a nursing student preparing for the NCLEX, it is crucial to have a solid understanding of diabetes and its pathophysiology. This article aims to provide an in-depth look at diabetes, including its types, causes, symptoms, and treatment methods. By grasping the fundamentals of diabetes, you will be better equipped to answer related questions on the NCLEX exam.
Types of Diabetes
There are three main types of diabetes: type 1, type 2, and gestational diabetes. Each type has distinct characteristics and underlying causes.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Type 1 Diabetes
Type 1 diabetes, also known as insulin-dependent diabetes mellitus (IDDM), is an autoimmune disorder. In this condition, the body's immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. As a result, the body is unable to produce insulin, leading to elevated blood glucose levels.
Type 1 diabetes typically develops in childhood or adolescence, although it can occur at any age. Patients with type 1 diabetes require lifelong insulin therapy to regulate their blood sugar levels.
Type 2 Diabetes
Type 2 diabetes, also known as non-insulin-dependent diabetes mellitus (NIDDM), is the most common form of diabetes. Unlike type 1 diabetes, type 2 diabetes is characterized by insulin resistance and impaired insulin secretion.
Insulin resistance occurs when the body's cells become less responsive to the effects of insulin. As a result, glucose is unable to enter the cells efficiently, leading to elevated blood sugar levels. Over time, the pancreas may also fail to produce enough insulin, further exacerbating the condition.
Type 2 diabetes is strongly associated with lifestyle factors such as obesity, sedentary behavior, and poor dietary choices. It often develops in adulthood, although the prevalence among children and adolescents is increasing.
Gestational Diabetes
Gestational diabetes occurs during pregnancy and affects approximately 2-10% of pregnant women. It is characterized by high blood glucose levels that develop during pregnancy and typically resolve after childbirth.
The exact cause of gestational diabetes is not fully understood, but hormonal changes and insulin resistance play a significant role. If left unmanaged, gestational diabetes can pose risks to both the mother and the baby. It increases the likelihood of complications during pregnancy and delivery and may predispose the mother to developing type 2 diabetes later in life.
Pathophysiology of Diabetes
To understand the pathophysiology of diabetes, it is essential to comprehend the role of insulin in the body. Insulin is a hormone produced by the beta cells in the pancreas. Its primary function is to regulate blood glucose levels by facilitating the uptake of glucose into cells.
In type 1 diabetes, the immune system attacks and destroys the beta cells, resulting in an absolute insulin deficiency. Without sufficient insulin, glucose cannot enter the cells, leading to hyperglycemia. The body compensates by breaking down fats for energy, causing the production of ketones. This can lead to a life-threatening condition called diabetic ketoacidosis (DKA).
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
In type 2 diabetes, insulin resistance is the primary issue. The body's cells become less responsive to insulin, impairing glucose uptake. Initially, the pancreas compensates by producing more insulin, but over time, it may become exhausted and fail to secrete enough insulin. This leads to persistently elevated blood glucose levels.
Gestational diabetes is thought to occur due to hormonal changes during pregnancy, which can lead to insulin resistance. The placenta produces hormones that interfere with insulin action, resulting in elevated blood glucose levels.
Symptoms and Complications
The symptoms of diabetes can vary depending on the type and severity of the condition. However, common symptoms include:
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow wound healing
- Recurrent infections
If left untreated or poorly managed, diabetes can lead to various complications, including:
- Cardiovascular disease
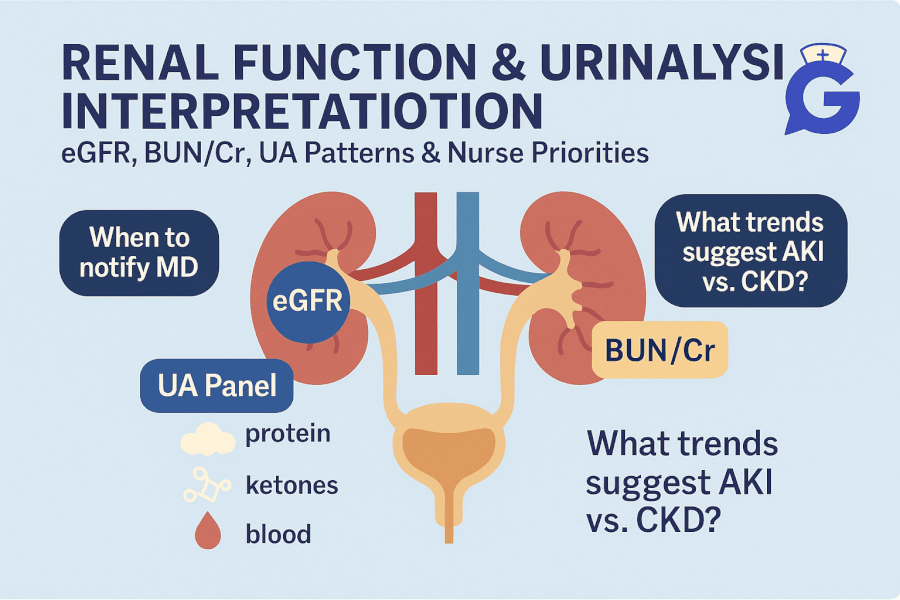
- Kidney disease
- Nerve damage (neuropathy)
- Eye damage (retinopathy)
- Foot complications (diabetic foot ulcers)
- Skin conditions (such as fungal infections)
Treatment and Management
The management of diabetes involves a combination of lifestyle modifications, medication, and regular monitoring. The primary goals of treatment are to maintain blood glucose levels within a target range, prevent complications, and improve quality of life.
For type 1 diabetes, insulin replacement therapy is essential. This involves administering insulin via injections or an insulin pump to mimic the body's normal insulin production. Additionally, individuals with type 1 diabetes must carefully monitor their blood glucose levels, count carbohydrates, and make appropriate adjustments to their insulin doses.
Type 2 diabetes management often begins with lifestyle modifications, such as adopting a healthy diet, increasing physical activity, and losing weight if necessary. Medications may also be prescribed to help control blood glucose levels. These medications can include oral antidiabetic drugs, injectable medications, or a combination of both.
Gestational diabetes is typically managed through dietary changes and regular physical activity. In some cases, insulin therapy may be necessary to maintain blood glucose levels within the target range.
Regular monitoring of blood glucose levels is crucial for all individuals with diabetes. This helps to assess the effectiveness of treatment and make necessary adjustments. Additionally, routine screening for complications, such as eye exams and kidney function tests, is recommended.
Conclusion
Understanding the pathophysiology of diabetes is vital for nursing students preparing for the NCLEX. By familiarizing yourself with the different types of diabetes, their causes, symptoms, and treatment methods, you will be better equipped to answer related questions on the exam. Remember to study the specific nursing interventions and considerations for patients with diabetes, as this knowledge will be invaluable in your nursing career.