When a lab flags potassium at 6.2 with peaked T waves, you don’t have time to hunt for scattered notes. In my years precepting step-down units, I’ve seen students freeze here. This guide gives you a calm, step-by-step plan for hyperkalemia: quick pathophysiology, priority nursing diagnoses, SMART outcomes, and interventions with rationales—including ECG safety, insulin/dextrose, beta-agonists, binders, and dialysis triggers. Use it for pre-conference, simulations, and real-time charting so you can act decisively and document like a pro.
Studying multiple electrolytes? Read our master hub:
The Ultimate Guide to Electrolyte Imbalances - frameworks, tables, and 20+ NGN micro-cases.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Pathophysiology of Hyperkalemia
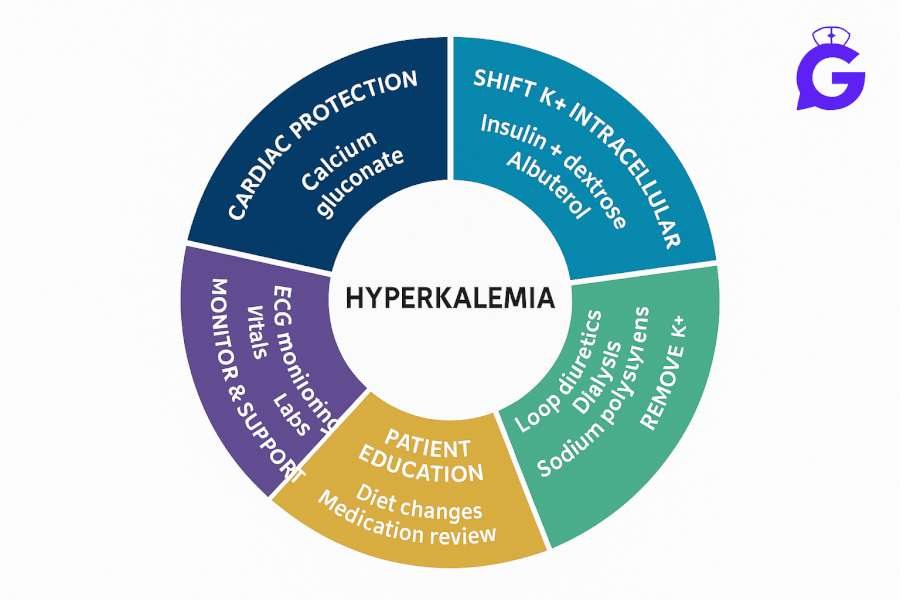
Hyperkalemia is typically defined by serum potassium > 5.0 mEq/L (institution ranges vary). Dangerous elevations reduce myocardial membrane excitability thresholds, producing peaked T waves, widened QRS, sine-wave patterns, and risk of ventricular arrest. Common drivers include decreased excretion (AKI/CKD), medications (ACEi/ARB, potassium-sparing diuretics, NSAIDs), tissue breakdown (rhabdomyolysis, tumor lysis), metabolic acidosis (K⁺ shifts out of cells), and high K⁺ intake or transfusions. Initial management prioritizes: 1) myocardial stabilization with IV calcium, 2) intracellular shift of K⁺ (insulin/dextrose, beta-agonist ± bicarbonate if acidotic), and 3) K⁺ removal (loop diuretics, binders, dialysis) while addressing the cause.
Sharpen clinical judgment with NGN cases: Med-Surg Physiological Adaptation and practice documentation language with ABG Interpretation: 15 Cases.
Nursing Care Plans for Hyperkalemia
Below are high-yield nursing diagnoses with SMART outcomes, interventions, and rationales to individualize for your patient.
Nursing Diagnosis: Risk for Decreased Cardiac Output (dysrhythmias)
| Category | Details |
|---|---|
| Related to | Altered myocardial conduction from elevated extracellular potassium |
| As evidenced by | Peaked T waves, widened QRS, brady/ventricular dysrhythmias; K⁺ above facility threshold |
| Desired Outcomes | Maintains stable rhythm (no VT/VF/asystole); ECG changes improve within 1–2 hours of therapy; K⁺ trends toward target per provider orders. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Place on continuous cardiac monitoring; obtain STAT 12-lead ECG; keep defibrillator accessible. | Detects life-threatening changes early and prepares for rapid response. |
| Administer IV calcium (gluconate/chloride) per protocol for ECG changes or severe K⁺ elevation. | Stabilizes cardiac membranes to reduce malignant dysrhythmias while other therapies act. |
| Hold exogenous potassium, potassium-sparing diuretics, ACEi/ARB, and NSAIDs as ordered. | Prevents further K⁺ elevation and supports correction. |
Nursing Diagnosis: Risk for Unstable Blood Glucose Level (insulin therapy for K⁺ shift)
| Category | Details |
|---|---|
| Related to | Insulin/dextrose therapy to shift K⁺ intracellularly; decreased intake during illness |
| As evidenced by | (Risk factors) IV insulin orders, NPO status, variable nutrition, renal impairment |
| Desired Outcomes | Blood glucose remains 100–180 mg/dL during therapy; no symptomatic hypoglycemia; K⁺ decreases per protocol within 1–2 hours. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Give regular insulin IV with dextrose per order; check glucose q15–30 min initially, then hourly x 3–4 hrs. | Lowers K⁺ by intracellular shift; close monitoring prevents/detects hypoglycemia. |
| Consider nebulized albuterol per order; give sodium bicarbonate if acidotic and ordered. | Beta-agonists and correction of acidosis enhance intracellular K⁺ shift. |
| Assess for rebound hyperkalemia after shifts; repeat labs per protocol. | Shifts are transient; ongoing checks ensure sustained correction. |
Nursing Diagnosis: Deficient Knowledge (hyperkalemia safety & prevention)
| Category | Details |
|---|---|
| Related to | New diagnosis; complex medication changes; renal disease; diet confusion |
| As evidenced by | Questions about diet, binders, diuretics, ACEi/ARB adjustments, and when to seek care |
| Desired Outcomes | Patient/family teach back home plan: med changes, binder timing, diet basics, lab follow-up, and red-flag symptoms. |
Nursing Interventions and Rationales
| Intervention | Rationale |
|---|---|
| Teach “3-step” approach: stabilize (IV calcium), shift (insulin/dextrose, albuterol, ± bicarbonate), remove (diuretics, binders, dialysis). | Clarifies why multiple therapies are used and what to expect. |
| Reinforce binder specifics if prescribed (e.g., sodium zirconium cyclosilicate/patiromer): timing with other meds/foods. | Optimizes efficacy and reduces interactions/constipation risk. |
| Provide diet basics individualized by provider (renal diet; avoid salt substitutes high in K⁺). | Reduces recurrent K⁺ load while maintaining nutrition. |
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
Frequently Asked Questions (FAQ)
What is the priority nursing action for hyperkalemia with ECG changes?
Protect the heart: initiate continuous monitoring and give IV calcium per protocol to stabilize the myocardium, then proceed with K⁺ shift/removal therapies as ordered.
Which interventions lower potassium fastest?
Insulin with dextrose (minutes) and nebulized albuterol shift K⁺ intracellularly. These are temporary—pair with removal (loop diuretics if making urine, potassium binders, or dialysis for severe CKD/AKI).
Do I ever give bicarbonate?
In metabolic acidosis with hyperkalemia, sodium bicarbonate may be ordered to help shift K⁺ intracellularly and correct pH. Follow facility protocols and monitor sodium/volume status.
Further Reading
- ABG Interpretation: 15 Practice Cases (with Rationale)
- NGN Med-Surg Case Studies: Physiological Adaptation
- Electrolyte Imbalances Made Easy: Mnemonics (2025)
- Electrolytes Cheat Sheet (2025): Na⁺/K⁺/Ca²⁺/Mg²⁺ Patterns
- Hypercalcemia Nursing Care Plan (2025)
- Hypocalcemia Nursing Care Plan (2025)
- Primary Hyperparathyroidism Nursing Care Plan (2025)
- Hypercalcemia of Malignancy Nursing Care Plan (2025)
- Calcium Kidney Stones (Nephrolithiasis) Nursing Care Plan (2025)