You don’t need to memorize every number - you need a repeatable way to turn labs and images into safe actions. This pillar brings together our most-used lab panels (CBC, CMP/electrolytes, coags, renal/UA, cardiac markers), high-yield tests (ABG, lactate), and bread-and-butter diagnostics (CXR, EKG, a-lines). For each, you’ll see: what it tells you, first actions, and parameters to recheck - the same NGN habit we teach across GoodNurse.
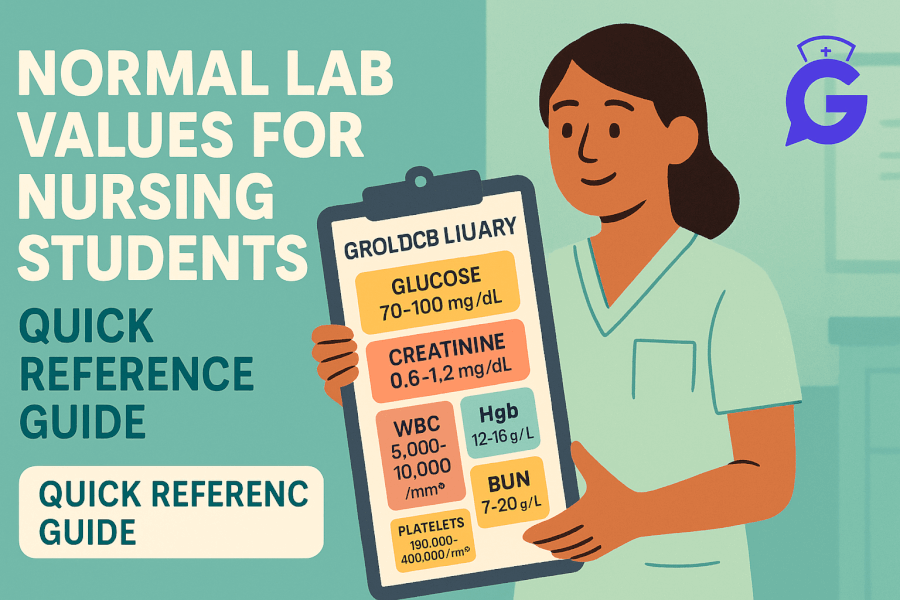
If you want quick values at your elbow, keep Normal Lab Values (2025) open while you read. For integrated practice, rotate through NGN Case Studies: 25 Free Examples with Answers.
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- How to Use This Guide (Action → Parameter)
- CBC & CMP: Ranges to Red Flags
- Electrolytes: Patterns & Nurse Actions
- Coagulation Studies: PT/INR, aPTT, D-dimer, Fibrinogen
- Renal Function & Urinalysis
- Cardiac Markers: Troponin & BNP
- ABG Interpretation (Stepwise)
- Lactate in Suspected Sepsis
- EKG Basics: Rhythm ID & First Actions
- Chest X-Ray ABCDE: What to Look For
- Arterial Lines & MAP
- NGN Study Strategy & Mini Practice
- FAQs
- Further Reading
How to Use This Guide (Action → Parameter)
- Name the priority (oxygenation, perfusion, bleeding risk, renal injury, electrolyte derangement).
- Choose two actions that change physiology now (oxygen, fluids, fix potassium, reposition, escalate).
- Pick two parameters you’ll recheck soon to prove it worked (SpO₂, RR/WOB, MAP, UOP, mentation, ECG).
Professor’s note: GoodNurse teaches this the same way I grade: you get full credit when your actions fix physiology and you pick the right parameters to verify it.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
CBC & CMP: Ranges to Red Flags
What they tell you
- CBC: oxygen-carrying capacity (Hgb/Hct), infection/inflammation (WBC), bleeding/clotting risk (platelets).
- CMP: electrolytes, renal markers (BUN/Cr), liver enzymes, glucose—your global “terrain map.”
First actions
- Anemia with symptoms: oxygen to target, minimize exertion, anticipate transfusion per order; trend Hgb and symptoms.
- Leukocytosis + sepsis picture: oxygen, fluids per order, cultures per policy.
- Low platelets + bleeding: pressure, minimize sticks, review meds/coags; notify quickly.
Recheck parameters
SpO₂, MAP, UOP, mentation, bleeding visibility, pain relief.
Deep dive when you need it: CBC & CMP (2025).
Electrolytes: Patterns & Nurse Actions
K⁺ drives rhythm; Na⁺ drives mentation; Ca²⁺/Mg²⁺ steady the myocardium/neuromuscular junctions.
- Hypokalemia: PVCs, U waves → replace per protocol, cardiac monitor, watch digoxin interactions.
- Hyperkalemia: peaked T, widened QRS → stabilize myocardium, shift/remove K⁺ per algorithm.
- Hyponatremia: confusion, seizures → safety first, manage sodium correction as ordered.
Recheck: ECG rhythm, mentation, K⁺/Na⁺/Mg²⁺ trend, symptoms.
Quick tables + actions: Electrolytes (2025).
Coagulation Studies: PT/INR, aPTT, D-dimer, Fibrinogen
Use: monitor anticoagulants, bleed/clot risk, DIC screens.
- High INR + bleeding: pressure, secure IV, anticipate reversal per order.
- Elevated aPTT on heparin: protocol-driven rate changes, bleeding watch.
- D-dimer: rule-out helper with low clinical probability; not a stand-alone diagnosis.
Actions → parameters: visible bleeding, MAP/HR, INR/aPTT trend.
Full walkthrough: Coagulation Studies (2025).
Renal Function & Urinalysis
BUN/Cr/eGFR + UA tell you perfusion vs intrinsic disease vs obstruction.
- Pre-renal AKI: high BUN:Cr, bland UA → restore perfusion, stop nephrotoxins, strict IOs.
- ATN: granular casts, fixed SG ~1.010 → remove insult, support perfusion.
- Pyelo/UTI: pyuria, nitrites/LE, WBC casts possible → culture per policy, antibiotics per order.
Parameters: UOP, MAP, Cr/eGFR, symptoms.
Full guide: Renal & UA Interpretation (2025).
Cardiac Markers: Troponin & BNP
- Troponin: myocardial injury pattern; trend with symptoms and EKG.
- BNP/NT-proBNP: volume/pressure overload; interpret with CXR and exam.
Actions: oxygen, monitor, IV access; escalate for ischemia/instability.
Parameters: pain, SpO₂, MAP, rhythm.
Time-course & thresholds: Cardiac Markers (2025).
ABG Interpretation (Stepwise)
- pH (acidic vs alkalemic).
- PaCO₂ (ventilation) and HCO₃⁻ (metabolic).
- Compensation pattern.
- PaO₂/SpO₂ (oxygenation).
- Clinical fit (WOB, perfusion, lactate).
Practice with answers: ABG Interpretation Made Simple (2025).
Lactate in Suspected Sepsis
A perfusion clue, not a verdict. Draw at suspicion and trend after interventions.
- Pitfalls: β-agonists, seizures, handling delays.
- If rising despite oxygen/fluids: escalate support and evaluate source control.
Parameters: SpO₂, MAP, UOP, mentation, ABG, lactate trend.
Bedside guide: Lactate in Sepsis (2025).
EKG Basics: Rhythm ID & First Actions
- Unstable (hypotension, altered mentation, chest pain): treat physiology first while you gather more data.
- AFib/flutter: rate vs rhythm control; anticoagulation assessment.
- SVT: vagal → adenosine per order if stable.
- Blocks: watch meds/electrolytes; prepare to pace if high-grade with instability.
- VT/VF: follow ACLS; defibrillate/cardiovert per algorithm.
Learn the fast checklist: EKG Basics (2025).
Electrolyte-rhythm ties: Electrolytes (2025).
Chest X-Ray ABCDE: What to Look For
- Airway: trachea midline? carina?
- Breathing: asymmetry, consolidation, PTX, effusions.
- Circulation: heart size (PA), edema patterns.
- Diaphragm: domes, free air, hernia.
- Everything else: bones, soft tissue, lines & tubes.
Walkthrough with examples: Chest X-Ray for Nurses (2025).
Arterial Lines & MAP
- Setup: pressurized flush, level at phlebostatic axis, zero correctly, square-wave test.
- Artifacts: over/under-damped waveforms mislead MAP—fix the system first.
- Targets: many aim for MAP ≥ 65 (follow team targets, confirm organ response).
Hands-on basics: Arterial Lines & MAP (2025).
NGN Study Strategy & Mini Practice
Study smarter
- Pair each lab/imaging concept with one case (bow-tie/matrix) where your action → parameter pair is obvious.
- Build mini-checklists: “If K⁺ high → stabilize, shift/remove; recheck ECG.” “If INR high + bleed → pressure, reversal plan; recheck INR/bleeding.”
Mini practice scenarios (answers collapsed)
1) Hyperkalemia + peaked T waves
- First actions: cardiac monitor, stabilize myocardium, shift/remove K⁺ per algorithm.
- Parameters: ECG QRS/T, K⁺ trend, symptoms.
2) Rising creatinine + oliguria
- First actions: stop nephrotoxins, restore perfusion, strict IOs; scan bladder if suspect obstruction.
- Parameters: UOP, MAP, Cr/eGFR.
3) Elevated INR with oozing at line site
- First actions: pressure, minimize sticks, notify; reversal plan per order.
- Parameters: visible bleeding, INR, MAP/HR.
4) “Bat-wing” edema on CXR + dyspnea
- First actions: oxygen, upright position; anticipate diuresis per plan.
- Parameters: SpO₂, RR/WOB, UOP, symptom relief.
5) Lactate up despite fluids & oxygen
- First actions: escalate perfusion support, evaluate source control.
- Parameters: MAP, UOP, lactate trend, ABG.
For full NGN examples with answers:
- NGN Med-Surg / Physiological Adaptation (2025)
- NGN Pediatrics & Psych (2025)
- NGN Pharmacology (2025)
FAQs
What should I trend with any “bad” lab?
Pick two parameters that will move soon: SpO₂, RR/WOB, MAP, UOP, mentation, ECG—then decide if your action worked.
How do I avoid anchoring on a single value?
Use the story + trend. Pair the lab with symptoms and repeat after your intervention.
Where should I put my time on NGN?
Practice action → parameter pairs and recognize red-flag patterns (hyperK ECG, rising lactate + low MAP, high INR + bleeding).