A 12-lead looks busy, but rhythm safety starts with a simple, repeatable checklist. In clinical and on NGN items, your job is to 1) name the priority, 2) choose two actions that change physiology, and 3) pick two parameters you’ll recheck soon to prove it worked. This guide gives you a friendly, stepwise approach to common rhythms and the first actions that keep clients safe.
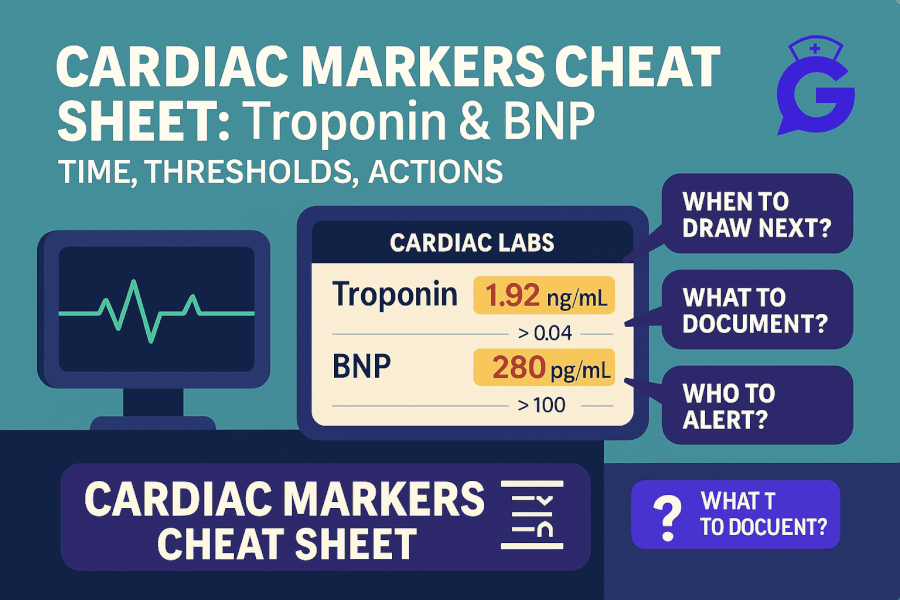
For context on perfusion labs and cardiorespiratory overlap, open Cardiac Markers (2025): Troponin & BNP and ABG Interpretation Made Simple (2025). If a case stem floods you with data, reset with How to Read NGN Case Stems (2025).
Table of Contents
- How to Read an EKG Fast (Floor Method)
- Sinus Rhythms
- Atrial Fibrillation & Flutter
- SVT (Narrow-Complex Tachycardia)
- AV Blocks (1st, 2nd, 3rd Degree)
- Ventricular Rhythms: VT & VF
- STEMI & Ischemia Clues (12-Lead Snapshots)
- NGN Tie-Ins: Action → Parameter Pairs
- Mini Practice Cases (with Answers)
- FAQs
- Further Reading
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
How to Read an EKG Fast (Floor Method)
Five checks, same order every time (use a 6-second strip if given):
- Rate: ~300/150/100/75/60/50 method or small-box math; confirm with monitor readout.
- Rhythm regularity: R-R distance regular or irregular?
- P waves: present and similar? One P before each QRS?
- PR interval: ~0.12–0.20 s and constant?
- QRS width: narrow (<0.12 s) or wide (≥0.12 s)? Look for bizarre morphology.
Red-flag overlay: If unstable (hypotension, altered mentation, chest pain, shock signs), treat physiology first while you gather more data.
Professor’s note: A beautiful interpretation with an unstable client is the wrong answer. Prioritize oxygenation, perfusion, and rapid escalation.
Sinus Rhythms
Normal sinus rhythm (NSR): Regular, P before each QRS, PR ~0.12–0.20 s, QRS narrow.
Sinus bradycardia: Rate < 60; common in athletes, during sleep, or with meds (β-blockers).
Sinus tachycardia: Rate > 100; think fever, pain, hypovolemia, hypoxia, anxiety.
Nursing priorities
- Brady + unstable? Oxygen, monitor, IV access; anticipate ACLS-guided therapy per orders.
- Tachy root cause: Treat hypovolemia (fluids), hypoxia (oxygen), pain/anxiety (per plan).
- Parameters: SpO₂, BP/MAP, mentation, symptoms.
For lab context when tachy/brady links to disease burden, see Electrolytes (2025) and Cardiac Markers.
Atrial Fibrillation & Flutter
AFib: Irregularly irregular R-R, no distinct P waves; variable rate.
AFlutter: Sawtooth flutter waves (best in II, III, aVF), typical atrial rate ≈ 300 with variable conduction.
Nursing priorities
- Unstable AFib/flutter (hypotension, altered mentation): Oxygen, monitoring, IV access; anticipate urgent rate/rhythm management.
- Stable with RVR: Rate control per orders; evaluate anticoagulation needs and stroke risk.
- Parameters: HR, BP/MAP, symptoms (dizziness, dyspnea), signs of poor perfusion.
Cross-check coag and bleeding considerations in Coagulation Studies (2025) and med-level nuances in Therapeutic Drug Levels (2025) (digoxin-related bradyarrhythmias).
SVT (Narrow-Complex Tachycardia)
Clues: Regular narrow-complex tachycardia, often 150–220 bpm; P waves hidden in prior T wave or retrograde.
Nursing priorities
- Unstable: Oxygen, monitoring, IV access; prepare for synchronized cardioversion per orders.
- Stable: Vagal maneuvers per protocol; anticipate adenosine per order (watch for flushing/chest pressure).
- Parameters: HR, BP/MAP, symptoms, rhythm response.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
AV Blocks (1st, 2nd, 3rd Degree)
First-degree: PR > 0.20 s, constant; usually benign, watch meds/electrolytes.
Second-degree Type I (Wenckebach): PR progressively lengthens until a beat drops.
Second-degree Type II: PR constant with random dropped QRS—can progress to 3rd-degree; watch for instability.
Third-degree (complete): Atria and ventricles dissociated; ventricular escape rhythm often slow/wide; perfusion risk is high.
Nursing priorities
- Oxygen, monitor, IV access; look for drug effects (β-blockers, CCBs, digoxin) and electrolyte issues (K⁺, Mg²⁺).
- Unstable high-grade block: anticipate pacing per team plan.
- Parameters: HR, BP/MAP, mentation; rhythm changes after interventions.
For electrolyte-rhythm interplay, see Electrolytes (2025) and for digoxin context, revisit Therapeutic Drug Levels (2025).
Ventricular Rhythms: VT & VF
Ventricular tachycardia (VT): Wide-complex tachycardia; monomorphic or polymorphic.
Ventricular fibrillation (VF): Chaotic, no organized QRS; no pulse.
Nursing priorities
- VT/VF pulseless: Start CPR and follow ACLS; ensure early defibrillation per protocol.
- VT with pulse (unstable): Prepare for synchronized cardioversion per orders.
- Parameters: Return of pulses, rhythm conversion, MAP, mentation.
STEMI & Ischemia Clues (12-Lead Snapshots)
- ST elevation in contiguous leads with reciprocal depression elsewhere suggests acute injury—treat as a time-critical emergency.
- Ischemia may show ST depression and/or T-wave inversion.
- Pair rhythm with symptoms + troponin trends (see Cardiac Markers). Don’t delay oxygen for hypoxemia, IV access, monitoring, and rapid team activation.
Professor’s note: On NGN, “Which action first?” usually means “Which action changes physiology now?” Oxygen for hypoxemia, synchronized cardioversion for unstable tachyarrhythmia, pacing readiness for unstable block.
NGN Tie-Ins: Action → Parameter Pairs
- Unstable AFib with RVR → actions: oxygen, prepare for urgent rate/rhythm control → parameters: HR, MAP, symptoms.
- SVT stable → actions: vagal maneuvers, prepare adenosine per order → parameters: rhythm conversion, symptoms, MAP.
- High-grade AV block with dizziness → actions: oxygen, pacing readiness → parameters: HR, MAP, mentation.
- VT/VF → actions: ACLS, defibrillation/cardioversion per algorithm → parameters: pulses, rhythm, MAP.
Mini Practice Cases (with Answers)
Case 1 — Irregularly Irregular
- Stem: 78-year-old with dyspnea; EKG shows irregularly irregular rhythm, no P waves, narrow QRS; BP 94/58.
- Question: First actions?
- Answer: Oxygen, monitor, IV access; rapid team evaluation for rate/rhythm control.
- Rationale: Unstable AFib; physiology first (SpO₂/MAP) before detailed interpretation.
Case 2 — Narrow, Regular at 190
- Stem: 24-year-old palpitations; narrow-complex tachycardia ~190; BP 108/66; mentation normal.
- Question: Priority sequence?
- Answer: Vagal maneuvers; prepare adenosine per order; monitor rhythm response.
- Rationale: Stable SVT pathway.
Case 3 — Dropped Beats
- Stem: 65-year-old dizzy; constant PR then random dropped QRS; HR 40; BP 86/54.
- Question: Next best step?
- Answer: Oxygen, IV access, pacing readiness; notify team.
- Rationale: Second-degree Type II can progress—prepare to pace.
Case 4 — Wide, Very Fast
- Stem: 58-year-old with chest discomfort; wide-complex tachycardia; pulses present; BP 76/44.
- Question: Best action?
- Answer: Prepare for synchronized cardioversion per orders; oxygen, monitoring.
- Rationale: Unstable VT with pulse.
Case 5 — STEMI Picture
- Stem: Crushing chest pain, diaphoresis; ST elevation in contiguous leads; reciprocal depression.
- Question: What proves your actions worked?
- Answer: Pain down, MAP stable, SpO₂ adequate, rhythm stable; troponin will trend later—don’t wait.
For integrated study structure and NGN stems across systems, see the NGN Case Studies hub and rotate practice with Med-Surg Physiological Adaptation.
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
FAQs
Is AFib always an emergency?
No. Focus on stability first. If hypotensive/altered, escalate rapidly; if stable, rate control and anticoagulation assessment follow policy.
How do I tell SVT from sinus tachycardia quickly?
SVT is typically very regular with hidden P waves and abrupt onset/termination. Treat the cause in sinus tachy; use vagal/adenosine pathway for stable SVT as ordered.
When do I worry about wide QRS?
Any new wide-complex tachycardia is concerning—treat as VT until proven otherwise and manage by stability.
Do electrolytes really change rhythms?
Yes—K⁺/Mg²⁺ shifts drive irritability and blocks. Review Electrolytes (2025) for patterns and nurse actions.