Infection control practices are a crucial topic that every aspiring nurse must be well-versed in for success on the NCLEX. The National Council Licensure Examination (NCLEX) is a standardized test that determines whether an individual is ready to begin practicing as a nurse.
Infection control is a foundational component of nursing practice, helping prevent the spread of infections in healthcare settings. This article provides a comprehensive NCLEX review of infection control practices, including standard precautions, transmission-based precautions, and the safe handling of infectious materials.
Standard Precautions: The First Line of Defense
Standard precautions are the cornerstone of infection control and should be applied to all patients, regardless of their infection status. These precautions help prevent the spread of bloodborne and other pathogens.
Key Components of Standard Precautions
-
Hand Hygiene
Hand hygiene is the single most effective way to prevent the spread of infection. Use soap and water when hands are visibly soiled or after contact with bodily fluids. Otherwise, alcohol-based hand rubs are acceptable. -
Personal Protective Equipment (PPE)
Gloves, gowns, masks, and eye protection should be worn based on the level of exposure. For example, gloves are necessary when there’s potential for contact with blood or body fluids. -
Respiratory Hygiene / Cough Etiquette
Encourage patients to cover coughs/sneezes with their elbow or a tissue. Provide masks to patients showing respiratory symptoms. -
Safe Injection Practices
Use a new needle and syringe for each injection. Never reuse single-dose vials. -
Handling of Equipment and Surfaces
Clean and disinfect equipment between patient uses. Properly dispose of contaminated items in labeled biohazard containers.
Transmission-Based Precautions: Additional Layers of Protection
In some cases, standard precautions are not enough. Transmission-based precautions are used for patients with known or suspected infections that are transmitted via contact, droplets, or airborne particles.
Contact Precautions
- Used for MRSA, C. diff, and similar pathogens.
- Requires gloves and gowns upon entry.
- Limit patient movement outside the room.
Droplet Precautions
- Used for illnesses like influenza or pertussis.
- Wear a surgical mask within 3 feet of the patient.
- Patient should wear a mask during transport.
Airborne Precautions
- Used for tuberculosis, measles, and varicella.
- Requires an N95 respirator and placement in a negative pressure room.
- Keep doors closed to maintain air integrity.
Handling of Infectious Materials: Proper Protocols Save Lives
Proper handling and disposal of infectious materials reduce cross-contamination and occupational risk.
1. Segregation and Disposal
- Dispose of sharps in puncture-resistant containers.
- Segregate biohazardous waste using red bags or containers.
2. Cleaning and Disinfection
- Follow manufacturer guidelines for disinfectants.
- Clean high-touch surfaces regularly using EPA-approved solutions.
3. Transportation of Infectious Materials
- Use leak-proof, labeled containers.
- Follow institution and CDC protocols for transporting lab specimens.
4. Spill Management
- Contain the spill immediately.
- Don appropriate PPE before cleaning.
- Use appropriate disinfectants and dispose of all cleaning materials as biohazard waste.
Tips for Answering Infection Control Questions on the NCLEX
Understanding the content is only half the battle — here are some smart strategies to apply during the NCLEX:
- Prioritize Safety: Think like a nurse — what action protects the patient or staff first?
- Watch for Red Flags: Misusing PPE, poor hand hygiene, or unsafe waste disposal are common traps.
- Apply Isolation Knowledge: Questions may test whether you know which disease fits which precaution type.
- Choose the Most Protective Answer: When in doubt, go with the most infection-preventing option.
Final Thoughts: Why Infection Control Matters
Infection control practices are not just rules — they’re patient-saving protocols that prevent healthcare-associated infections (HAIs). Mastering this content for the NCLEX demonstrates your readiness to keep both your patients and your coworkers safe. Remember: every nurse is responsible for infection prevention.
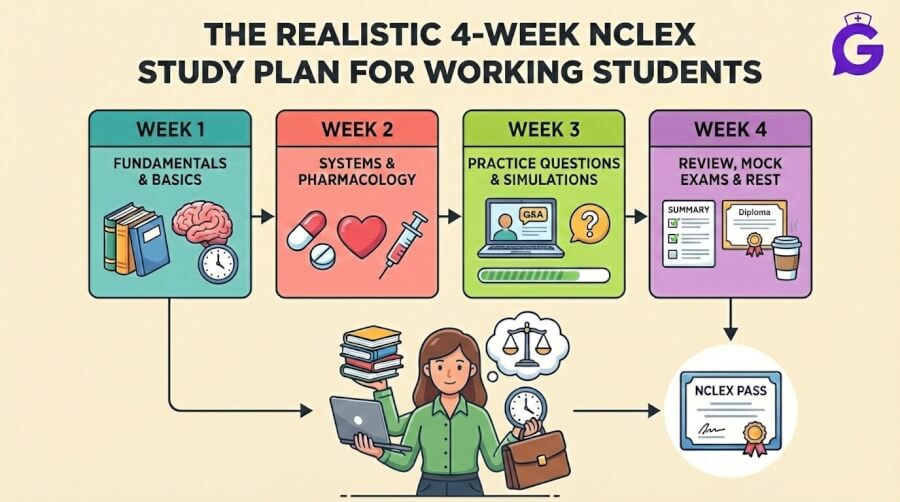
More NCLEX Prep Articles You’ll Find Helpful
Looking to reinforce your understanding or test your knowledge? Check out these must-read articles from GoodNurse:
- 25 Must-Know NCLEX Vocabulary Terms for 2025
- Common NCLEX Questions and Answers: A Comprehensive Review
- Next Gen NCLEX Case Studies: 25 Practice Questions with Answers
- NCLEX Categories Explained (2025): What Every Nursing Student Should Know
- NCLEX Vocabulary: 20 Essential Nursing Terms to Master with Questions (2025 Guide)