Introduction
Delirium Tremens (DTs) is a severe form of alcohol withdrawal that can be life-threatening if not properly managed. As a nursing student preparing for the NCLEX, understanding the pathophysiology, clinical presentation, and management of Delirium Tremens is crucial. This comprehensive guide will provide you with the essential knowledge needed to tackle NCLEX questions related to DTs, along with nine challenging practice questions to test your understanding.
💡 Ultimate NCLEX Study Mega Guide
Your must‑have resource to NCLEX cheat sheets, mnemonics & key topics - all in one place.
What is Delirium Tremens?
Delirium Tremens is a rapid onset of severe confusion and changes in the brain caused by withdrawal from alcohol. It typically occurs in individuals with a history of heavy alcohol use who suddenly stop drinking. DTs can manifest within 48-96 hours after the last drink and can last for 1-5 days.
Pathophysiology
The pathophysiology of DTs involves a complex interplay of neurotransmitter imbalances. Chronic alcohol use enhances the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) and inhibits the excitatory neurotransmitter glutamate. When alcohol intake is abruptly stopped, this balance is disrupted, leading to a hyperexcitable state in the central nervous system.
Risk Factors
- History of heavy alcohol use
- Previous episodes of alcohol withdrawal
- Concurrent medical conditions
- Older age
- Co-occurring psychiatric disorders
Clinical Presentation
- Severe agitation and confusion
- Hallucinations (visual, auditory, or tactile)
- Tremors
- Tachycardia
- Hypertension
- Fever
- Diaphoresis
- Seizures
Management of Delirium Tremens
Initial Assessment
- Comprehensive history and physical examination
- Assessment of vital signs
- Mental status examination
- Laboratory tests (electrolytes, liver function tests, complete blood count)
Pharmacological Management
- Benzodiazepines: First-line treatment to control agitation and prevent seizures. Commonly used benzodiazepines include diazepam, lorazepam, and chlordiazepoxide.
- Antipsychotics: May be used to manage severe agitation and hallucinations. Haloperidol is commonly used.
- Thiamine: Administered to prevent Wernicke's encephalopathy, a complication of chronic alcohol use.
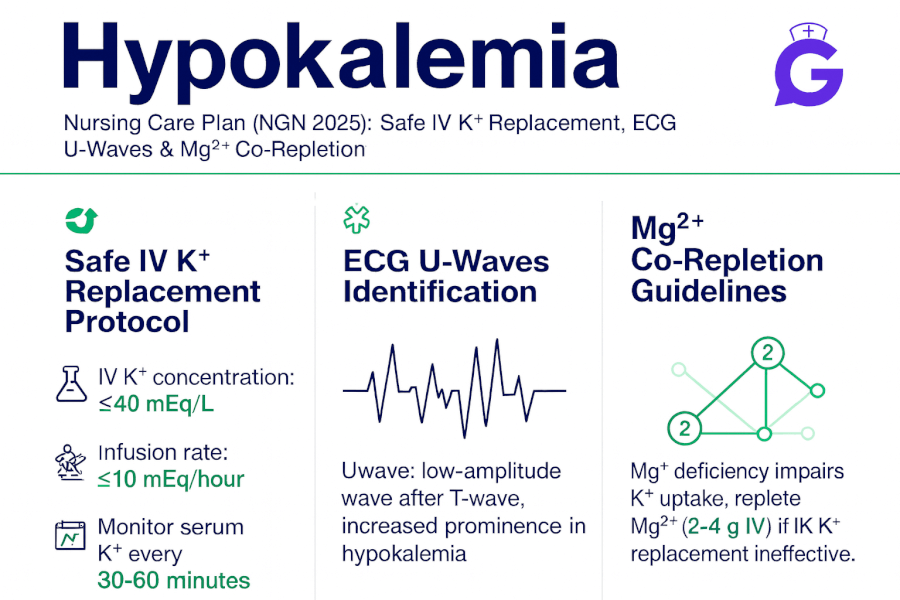
- Intravenous fluids: To correct dehydration and electrolyte imbalances.
- Magnesium sulfate: May be used to prevent seizures in patients with low magnesium levels.
Supportive Care
- Continuous monitoring of vital signs
- Ensuring a safe environment to prevent injury
- Nutritional support
- Psychological support and reassurance
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
NCLEX Practice Questions
Question 1
A 45-year-old male with a history of chronic alcohol use presents to the emergency department with confusion, tremors, and hallucinations. He last consumed alcohol 72 hours ago. What is the most appropriate initial treatment?
A. Haloperidol
B. Lorazepam
C. Thiamine
D. Magnesium sulfate
Answer: B. Lorazepam
Question 2
Which of the following is a hallmark sign of Delirium Tremens?
A. Bradycardia
B. Hypotension
C. Severe agitation and confusion
D. Hyperglycemia
Answer: C. Severe agitation and confusion
Question 3
What is the primary neurotransmitter imbalance involved in Delirium Tremens?
A. Increased dopamine
B. Decreased serotonin
C. Decreased GABA and increased glutamate
D. Increased acetylcholine
Answer: C. Decreased GABA and increased glutamate
Question 4
A patient with Delirium Tremens is at risk for which of the following complications?
A. Hypothermia
B. Seizures
C. Hypoglycemia
D. Bradycardia
Answer: B. Seizures
Question 5
Which of the following medications is administered to prevent Wernicke's encephalopathy in patients with Delirium Tremens?
A. Diazepam
B. Thiamine
C. Haloperidol
D. Magnesium sulfate
Answer: B. Thiamine
Question 6
A patient with Delirium Tremens is receiving intravenous fluids. Which electrolyte imbalance is most critical to monitor?
A. Hyperkalemia
B. Hypocalcemia
C. Hyponatremia
D. Hypomagnesemia
Answer: D. Hypomagnesemia
Question 7
What is the typical time frame for the onset of Delirium Tremens after the last drink?
A. 6-12 hours
B. 12-24 hours
C. 24-48 hours
D. 48-96 hours
Answer: D. 48-96 hours
Question 8
Which of the following is NOT a common symptom of Delirium Tremens?
A. Hallucinations
B. Tachycardia
C. Diaphoresis
D. Hypotension
Answer: D. Hypotension
Question 9
In managing a patient with Delirium Tremens, which of the following is the priority nursing intervention?
A. Administering antipsychotic medication
B. Ensuring a safe environment
C. Providing nutritional support
D. Monitoring liver function tests
Answer: B. Ensuring a safe environment
Conclusion
Delirium Tremens is a critical condition that requires prompt recognition and management. As you prepare for the NCLEX, understanding the pathophysiology, clinical presentation, and treatment options for DTs is essential. Use the practice questions provided to test your knowledge and ensure you are well-prepared to handle questions related to Delirium Tremens on the exam. Remember, thorough preparation and a solid understanding of key concepts are the keys to success on the NCLEX. Good luck!