If you can quickly decide who to see first, what to do next, and what to delegate, you’ll crush the NCLEX - and your first year on the floor. This guide gives you a repeatable decision framework, targeted examples, and rapid-fire mini-scenarios so you can practice clinical judgment under time pressure. The goal: lock in safety decisions that stand up on exam day and at the bedside.
For deeper lab/imaging context while you triage, keep Nursing Labs & Diagnostics (2025): Complete Guide + Cheat Sheets open. To tighten your stem-reading speed, review How to Read NGN Case Stems (2025). When drips enter the picture, double-check rate math with IV Drip Rates & Infusions (2025).
🎯 Free NCLEX quiz!
Test your knowledge - new quizzes added weekly!
Table of Contents
- The 5-Step Prioritization Framework
- Delegation Rules: RN vs LPN/VN vs UAP
- High-Yield Red-Flag Words on NCLEX
- Your First Look Checklist at the Bedside
- 25 Mini-Scenarios with Answers
- Common Traps & How to Beat Them
- Rapid Delegation Do/Don’t Table
- Key Takeaways
- FAQs
- Further Reading
🥇Voted #1 Nursing Study Tool.
Personalized AI Tutor + Instant Answers to All Your Questions. 100% Money Back Guarantee!
The 5-Step Prioritization Framework
1) Identify the core threat: ABCs + Safety.
Look for Airway obstruction (stridor, inability to speak), Breathing distress (RR, SpO₂, work of breathing), Circulation compromise (MAP, bleeding, syncope). Add Safety risks (active suicidal ideation, elopement, uncontrolled pain with VS changes, sepsis clues).
2) Classify: Acute vs. Chronic; Unstable vs. Stable.
Acute + Unstable outranks Chronic + Stable. Words like “new,” “sudden,” “recent change,” “post-op day 0–1,” “in the last hour” upgrade priority.
3) Predictable vs. Unpredictable trajectory.
A predictable issue (e.g., day-3 cellulitis improving) ranks below unpredictable/rapid decompensation (e.g., GI bleed with falling H/H).
4) Time-sensitive interventions first.
Narrow windows: insulin with BG changes, symptomatic bradycardia, chest pain with unstable ECG, tPA complications, active hemorrhage.
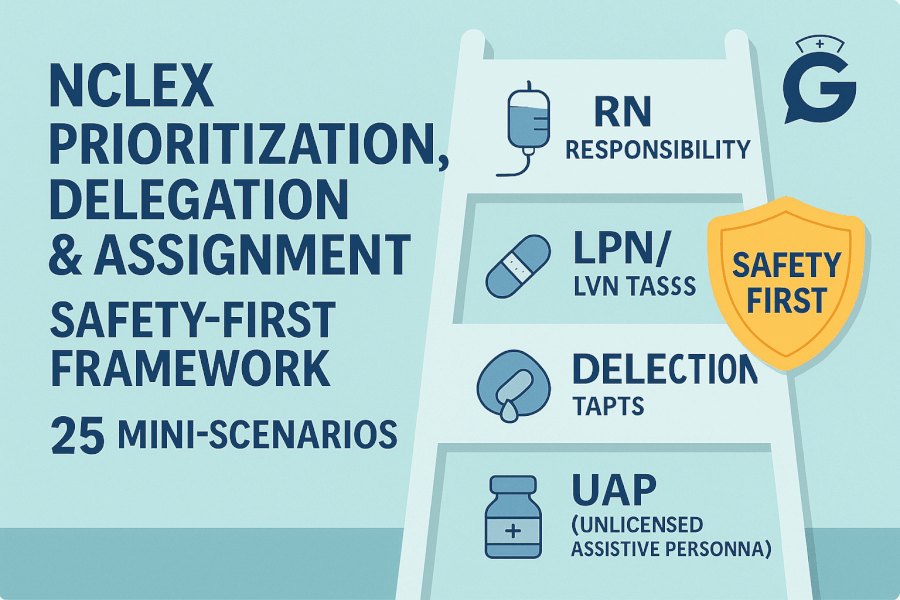
5) Delegate safely using “A-T-E.”
If the task is Assessment, Teaching, or Evaluation, it’s the RN. Save stable + predictable care for LPN/VN, and non-invasive ADLs for UAP (policy/state dependent).
For labs/imaging that often appear in stems, scan trends in Nursing Labs & Diagnostics and oxygenation/perfusion signals in ABG Interpretation Made Simple (2025).
Delegation Rules: RN vs LPN/VN vs UAP
RN (always retains):
- Initial assessments, admissions, discharges, care plans, triage, critical thinking decisions.
- Teaching (initial/new) and evaluation of outcomes.
- High-risk tasks: blood transfusion initiation/verification (policy), IV pushes for high-alert meds (policy), central line care.
LPN/VN (typical; check state/facility):
- Focused ongoing assessments on stable patients.
- Reinforce established teaching.
- Give most PO/IM/SQ meds; some IVPB meds per policy.
- Sterile procedures (e.g., dressings, Foley insertion) if allowed.
UAP (unlicensed assistive personnel):
- ADLs (bathing, grooming, feeding without aspiration risk).
- Ambulation, vitals on stable patients, I&O, glucose checks (if trained), non-sterile specimens.
Never delegate: A-T-E, unstable patients, new onset symptoms, triage, titrations, or any task requiring nursing judgment.
High-Yield Red-Flag Words on NCLEX
“Stridor,” “new confusion,” “RR 8,” “SpO₂ 86% RA,” “rigid abdomen,” “hematemesis,” “diaphoretic chest pain,” “MAP < 65,” “fever in neutropenia.”
These push a stem to see first. Confirm with ABCs and vitals; escalate.
Your First Look Checklist at the Bedside
- Vitals/monitor: RR, SpO₂, HR/rhythm, BP/MAP.
- Airway/appearance: Can they speak full sentences? Tripod? Cyanosis?
- Perfusion: Mental status, skin temp, cap refill, urine output trends.
- Lines/drips: Access patency, active vasoactive/insulin drips (verify orders/rates).
- Immediate action: Oxygen, position, notify/escalate, STAT labs per protocol, then reassess.
25 Mini-Scenarios with Answers
Format: Scenario → Who first? / Delegate? / Action? → Rationale
-
Post-thyroidectomy, new hoarseness + stridor.
See first. Do not delegate. Prepare to secure airway; notify provider; anticipate calcium check.
Rationale: Airway threat. -
COPD on 2 L O₂, baseline dyspnea unchanged, wants bath.
Lower priority. Delegate bath to UAP; RN reassesses later.
Rationale: Chronic + stable. -
Dementia patient rising from bed repeatedly.
Higher priority (safety). Delegate observation to UAP; RN addresses pain/toileting triggers.
Rationale: Fall risk. -
DKA on insulin drip; BG 58 mg/dL, diaphoretic.
See first. RN treats hypoglycemia per protocol.
Rationale: Time-sensitive. -
Neutropenic chemo patient; temp 100.9°F (38.3°C).
See first. RN initiates sepsis workup per protocol.
Rationale: Fever in neutropenia = emergency. -
New colostomy day 2, discharge teaching in 3 hrs.
RN (teaching/evaluation).
Rationale: A-T-E belongs to RN. -
Hip replacement POD#3; pain 7/10; stable VS; PRN due.
LPN may give PO PRN per policy; RN prioritizes unstable patients.
Rationale: Stable + predictable. -
Fresh trach 2 hrs ago; cuff leak alarm.
See first. RN assesses airway; keep trach kit/suction ready.
Rationale: Airway risk. -
HF exacerbation: new crackles, +2 kg overnight, SpO₂ 89% RA.
See first. RN: O₂, elevate HOB, anticipate diuresis.
Rationale: Acute decompensation. -
C. difficile patient needs CT transport.
Delegate transport to UAP with contact precautions; RN coordinates.
Rationale: Task-appropriate. -
Surgical incision with small stable drainage.
Lower priority. LPN can reinforce dressing, report changes.
Rationale: Predictable. -
Chest pain to jaw, diaphoretic, cool clammy skin.
See first. RN: rapid ECG, MONA per protocol, possible RRT.
Rationale: ACS risk. -
Acute ischemic stroke on tPA; new severe headache, ↑BP.
See first. RN: stop infusion, notify provider per protocol.
Rationale: Intracranial hemorrhage red flag. -
Post-op day 1 with rigid, board-like abdomen.
See first. RN: suspect peritonitis/bleed; NPO; escalate.
Rationale: Life-threatening. -
New confusion, RR 10 after opioids.
See first. RN: Airway/Breathing support; consider naloxone per order.
Rationale: Hypoventilation. -
Stable trach patient requests suctioning.
RN or LPN (if scope allows) performs; not UAP.
Rationale: Sterile airway procedure. -
Warfarin discharge teaching; today’s INR 1.9.
RN teaches and evaluates understanding.
Rationale: Teaching + evaluation. -
Psych: patient states active plan for self-harm.
See first. RN initiates 1:1 and safety protocol; notify provider.
Rationale: Immediate safety. -
T1DM requests HS snack; BG 122 mg/dL.
Delegate snack to UAP; RN monitors plan.
Rationale: Stable task. -
New cast; severe pain, pale toes, weak pulses.
See first. RN: evaluate for compartment syndrome; escalate.
Rationale: Limb-threatening. -
New PEG tube—initial assessment & first feed.
RN performs; later LPN can manage routine feeds.
Rationale: Initial assessment. -
Pneumonia stable on O₂ 2 L; needs IS teaching.
RN provides initial teaching; LPN reinforces later.
Rationale: Teaching ownership. -
Post-op wants early ambulation; VS stable.
Delegate assist/ambulation to UAP; RN confirms orders.
Rationale: Non-invasive, predictable. -
O₂ sat reads 82% but patient converses comfortably.
Assess patient first; verify probe placement/perfusion; UAP can warm hands/replace probe.
Rationale: Validate equipment. -
GI bleed: dark red stools, HR 122, dizzy on standing.
See first. RN: large-bore IVs per orders, labs, anticipate transfusion.
Rationale: Circulatory instability.
Common Traps & How to Beat Them
“Chronic” with a hidden change.
Chronic back pain? Lower priority. But “now radiating with numbness/incontinence” = urgent neuro eval.
Delegating embedded assessment.
“Feed dysphagia patient.” No—aspiration risk requires RN assessment.
“Ambulate day-0 hip replacement first time.” RN assesses first.
Stable ≠ titratable.
If vasoactives/insulin titration or central line care is involved, keep with RN, even if the patient looks “stable.”
Admission vs discharge.
Admissions often rank above discharges due to initial assessment/triage needs.
Vital sign bias.
Numbers need context. A COPD SpO₂ 90% may be baseline; RR 8 is more dangerous than a single BP 88/60 in an asymptomatic chronic patient—Airway/Breathing first.
Rapid Delegation Do/Don’t Table
| Task | UAP | LPN/VN | RN |
|---|---|---|---|
| ADLs, grooming, feeding (no aspiration risk) | ✅ | ✅ | ✅ |
| Vitals on stable patients | ✅ | ✅ | ✅ |
| Clean-catch urine specimen | ✅ | ✅ | ✅ |
| Glucometer checks (policy) | ✅ | ✅ | ✅ |
| Initial assessment/admission | ❌ | ❌ | ✅ |
| Teaching (initial/new) | ❌ | ❌ | ✅ |
| Reinforce prior teaching | ❌ | ✅ | ✅ |
| IV titration/vasoactives | ❌ | ❌ (usually) | ✅ |
| Blood transfusion start/verify | ❌ | ❌ (usually) | ✅ |
| Foley insertion, wound care (sterile)* | ❌ | ✅* | ✅ |
* if allowed by state/facility scope.
Key Takeaways
- Prioritize ABCs + Safety, then Acute/Unstable > Chronic/Stable and Time-sensitive first.
- Keep A-T-E (Assessment, Teaching, Evaluation) with the RN.
- LPN/VN = stable + predictable; UAP = non-invasive ADLs on stable clients.
- Watch for red-flag words: stridor, RR < 10, rigid abdomen, hematemesis, fever in neutropenia, MAP < 65.
- Practice speed: underline threats, mark scope, pick the first physiologic action, then verify with parameters.
FAQs
Can UAP take vitals on an unstable patient?
No. Unstable assessments remain with the RN; UAP can record vitals on stable patients per policy.
Can an LPN perform initial assessments?
Typically no—initial assessments/admissions are RN. LPNs can do focused ongoing assessments on stable clients (state/facility dependent).
Can an LPN reinforce discharge teaching?
Yes—reinforcement is appropriate. Initial/new teaching and evaluation remain RN.
Quickest way to rank four patients?
Scan ABCs, spot acute/unstable phrases, check time-sensitive meds/labs, then verify scope for delegation.
If two are both ABC threats?
Choose the one with a reversible intervention now (e.g., airway obstruction) or faster decompensation trajectory.