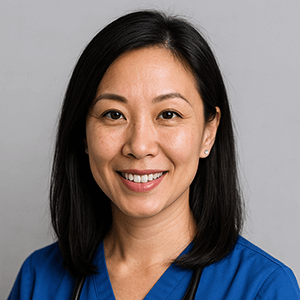
Digoxin toxicity is one of the most tested (and most clinically important) medication safety topics in nursing pharmacology. The reason is simple: digoxin has a narrow therapeutic index, meaning the difference between a therapeutic dose and a harmful dose can be small—especially in patients with electrolyte imbalances or renal impairment.
If you’re studying for the NCLEX-RN, NCLEX-PN, or reviewing cardiovascular medications for practice, this guide will help you:
- Understand what cardiac glycosides are and why digoxin is prescribed
- Explain digoxin’s mechanism of action in clear nursing language
- Identify high-yield nursing assessments before administration (including apical pulse parameters)
- Recognize early and late signs of digoxin toxicity
- Understand the role of potassium (and why hypokalemia is a red-flag risk factor)
- Know what happens next clinically, including Digoxin Immune Fab (Digibind/DigiFab)
- Walk away with NCLEX-ready “clinical pearls” and a quick self-check quiz
If you want a broader pharmacology foundation first, start with Mastering Pharmacology for the NCLEX (Comprehensive Guide) or the NCLEX Pharmacology Crash Course (7 Must-Know Concepts).
👉 Practice now with Cardiac Medications NCLEX Practice Questions.
What Are Cardiac Glycosides?
Cardiac glycosides are medications that improve cardiac performance by:
- Increasing myocardial contractility (positive inotropic effect)
- Slowing heart rate (negative chronotropic effect), especially by decreasing AV node conduction
The prototype drug you’ll see in nursing school and on the NCLEX is Digoxin (Lanoxin).
Primary clinical uses of digoxin
Digoxin is most commonly used for:
- Heart failure (especially when other therapies are insufficient or in select cases)
- Atrial fibrillation for ventricular rate control (slows AV node conduction)
For a broader cardiovascular medication overview, see NCLEX Cardiovascular Drugs: In-Depth Review (ACE inhibitors to Amiodarone).
Mechanism of Action: How Digoxin Works
Digoxin is a “two-for-one” medication conceptually:
- It increases squeeze (contractility)
- It slows conduction through the AV node (heart rate control)
Inotropic vs. chronotropic effects (nursing translation)
- Positive inotrope = stronger contraction = better cardiac output
- Negative chronotrope = slower heart rate = improved ventricular filling and rate control (especially helpful in A-fib)
If you need rhythm recognition support, pair this with EKG Basics for Nurses: Rhythm ID + Red Flags + First Actions or the faster visual-style review Cardiac Arrhythmias Cheat Sheet (NCLEX EKGs).
The sodium-potassium ATPase pump (what you must know)
Digoxin inhibits the sodium-potassium ATPase pump.
This leads to:
- Increased intracellular sodium
- Reduced sodium-calcium exchange
- Increased intracellular calcium
- Stronger myocardial contraction (positive inotropy)
This mechanism is also why electrolyte shifts—especially potassium—matter so much.
Potassium and digoxin compete at the cellular level.
Low potassium = higher digoxin effect = higher toxicity risk.
To lock in the electrolyte side of the concept, review:
- Electrolyte Imbalances Made Easy (Signs, Symptoms, Mnemonics)
- Electrolytes Cheat Sheet (Na/K/Ca/Mg/Phos Patterns + Nurse Actions)
- The Ultimate Guide to Electrolyte Imbalances (Patterns, Labs, NGN Decisions, Care Plans)
Nursing Assessment & Administration (What NCLEX Wants)
Digoxin is a classic medication-safety question on exams because it forces you to combine:
- Vital signs
- Rhythm assessment
- Lab values
- Patient symptoms
- Risk factors (age, renal function, electrolyte imbalance)
1) Check the apical pulse for 1 full minute
This is non-negotiable. Don’t shortcut it.
Hold parameters (common nursing school rules):
- Adults: hold if HR < 60 bpm
- Pediatrics: hold if HR < 90 bpm (school/facility dependent; always follow protocol)
If your site uses HR thresholds plus rhythm qualifiers (e.g., bradycardia with symptoms), the safe move is:
- Hold
- Assess
- Notify provider per protocol
2) Know the therapeutic range and timing
Digoxin is a “narrow window” drug, and therapeutic drug monitoring matters.
Your students will see ranges like 0.5–2.0 ng/mL in many nursing resources. Clinically, many settings prefer lower targets depending on the indication and patient factors, but for NCLEX you must know:
- Narrow therapeutic index
- Levels must be interpreted with symptoms, potassium, and renal function
For a broader “drug levels + toxicity + teaching” framework (including digoxin), use:
3) Evaluate renal function
Digoxin is largely cleared renally. When renal function declines:
- Digoxin can accumulate
- Toxicity risk rises, even at “normal” doses
If you want a labs-first way to reinforce this with students, link them to:
4) Pull in labs intelligently (don’t memorize blindly)
Digoxin questions often hinge on whether the nurse recognizes an abnormal lab trend.
Review:
Digoxin Toxicity: Recognition and Management
A high-yield way to teach digoxin toxicity is to group symptoms into three buckets:
- GI (early)
- Neuro/visual (classic)
- Cardiac dysrhythmias (dangerous)
Early signs (GI symptoms)
These are often the first warning signs:
- Nausea
- Vomiting
- Anorexia
- Abdominal pain
If the NCLEX stem says: “Patient has decreased appetite + nausea + is taking digoxin,” your brain should immediately think: possible toxicity → assess pulse, labs, symptoms.
Neurological and visual changes
Classic hallmark:
- Yellow-green halos (visual disturbances)
Other neuro symptoms:
- Confusion
- Dizziness
- Fatigue
- Weakness
Cardiac dysrhythmias (priority risk)
This is where digoxin becomes dangerous.
Potential findings:
- Bradycardia
- AV block / heart block
- PVCs
- Ventricular dysrhythmias (in severe toxicity)
If you want a rhythm-first refresher (especially for “what do I do first?” questions), revisit:
- EKG Basics for Nurses (Red Flags + First Actions)
- Cardiac Arrhythmias Cheat Sheet (Recognize + Treat)
Risk Factors for Digoxin Toxicity (NCLEX High-Yield)
Digoxin toxicity is less about “one wrong dose” and more about a patient who becomes vulnerable.
1) Hypokalemia (the #1 testable risk factor)
Hypokalemia increases digoxin’s effect at the cellular level.
Common causes:
- Loop diuretics (e.g., furosemide)
- Poor intake
- GI losses (vomiting/diarrhea)
- Inadequate replacement
To reinforce this with NGN-style decision-making, use:
- Hypokalemia Nursing Care Plan (Safe IV K replacement + ECG changes)
- Hyperkalemia Nursing Care Plan (First-hour priorities + ECG changes)
2) Renal impairment
Declining renal function reduces clearance → accumulation.
3) Drug-drug interactions
Common interaction patterns include:
- Amiodarone (can increase digoxin levels)
- Certain diuretics (indirectly via hypokalemia)
- Other agents affecting renal function or conduction
For a medication-class framework that helps students spot these patterns, use:
Medical Management & Antidotes (What Happens Next)
When toxicity is suspected, the typical clinical flow is:
- Hold digoxin
- Assess vital signs + symptoms
- Check labs (digoxin level, potassium, magnesium, renal function)
- Place on cardiac monitoring if indicated
- Treat underlying contributors (often electrolytes)
Digoxin Immune Fab (Digibind / DigiFab)
This is the antidote for severe/life-threatening toxicity.
Common indications include:
- Life-threatening dysrhythmias
- Hemodynamic instability
- Significant toxicity with high levels (context dependent)
Even if NCLEX doesn’t force you to know every dosing nuance, it will test:
- Recognition of toxicity
- Priority actions
- Safety steps (monitoring, labs, holding med)
To cement “therapeutic level vs toxicity vs teaching,” link again to:
NCLEX Clinical Pearls: What You Must Remember
Pearl 1: Don’t give digoxin without checking the apical pulse
If the question asks: “What should the nurse do first?” Apical pulse assessment is a top contender.
Pearl 2: Hypokalemia is a toxicity amplifier
Many NCLEX items are “two-step” logic:
- Patient on digoxin
- Patient has hypokalemia → toxicity risk is high.
Pearl 3: GI symptoms can be the earliest clue
Don’t ignore nausea/anorexia in a digoxin patient.
Pearl 4: Visual changes are classic
Yellow-green halos are the classic board-style clue.
Pearl 5: Dysrhythmias are the danger zone
When a stem includes bradycardia, blocks, PVCs, or dizziness/syncope: think safety + monitoring + escalation.
If you ever feel “lost” in pharmacology questions, re-center on three anchors:
Vitals → Labs → Symptoms.
That framework alone prevents a ton of NCLEX mistakes.
Quick Study Table (Save This)
| Concept | What to Remember |
|---|---|
| Drug class | Cardiac glycoside |
| Main uses | HF (select cases), A-fib rate control |
| Key nursing assessment | Apical pulse for 1 full minute |
| Hold parameter (common) | HR < 60 bpm (adult) |
| Therapeutic window | Narrow therapeutic index (levels + symptoms + labs) |
| Early toxicity | GI symptoms (nausea, vomiting, anorexia) |
| Classic clue | Yellow-green halos / blurred vision |
| Major risk factor | Hypokalemia |
| Antidote | Digoxin Immune Fab (Digibind/DigiFab) |
Check Your Knowledge (3 Questions)
-
A patient on digoxin reports nausea and has an apical pulse of 54 bpm. What is the nurse’s best first action?
-
Why does hypokalemia increase digoxin toxicity risk?
-
Which symptom is the most “classic” for digoxin toxicity on nursing exams?
Answer key (quick):
- Hold digoxin, assess symptoms, follow protocol/notify provider; check labs as ordered.
- Low potassium increases digoxin effect at the cellular level (higher binding/greater effect).
- Yellow-green halos / visual disturbances.
Further Reading (GoodNurse Internal Links)
- NCLEX Cardiovascular Drugs: In-Depth Review
- Electrolyte Imbalances Made Easy (Mnemonics + Symptoms)
- Therapeutic Drug Levels (Includes Digoxin)
- EKG Basics for Nurses (Rhythm ID + First Actions)
- Cardiac Medications NCLEX Practice Questions
References (High-Authority)
- NCSBN NCLEX-RN / NCLEX-PN Test Plans (Medication safety + Pharmacological and Parenteral Therapies): https://www.ncsbn.org
- American Nurses Association (Scope and Standards of Practice): https://www.nursingworld.org
- The Joint Commission (Medication safety / high-alert best practices): https://www.jointcommission.org